What is Venous Angioplasty and Stenting?
Narrowed or blocked large veins can cause severe swelling and pain. Venous angioplasty is a procedure done to treat these blockages. In some cases, a metal mesh tube called a stent may then be placed into the vein to hold it open. The procedure is done by a specially trained doctor like Dr. Jamnadas.
Venous blockages prevent the blood from draining out of the legs. Therefore the legs experience edema or swelling. In addition to the swelling, one can experience discomfort on walking, heaviness in the legs, and in severe cases, the skin turns brown, hard, cracks, and even ulcers can occur. Venous ulcers are extremely difficult to heal. This can be very debilitating. Therefore the treatment of venous disease is very important. This means of relieving the venous blockage so that the blood can come out of the leg, decompressing the leg and relieve symptoms.
Patients with previous blood clots in the legs are particularly prone to stenosis in the veins (narrowing). Other patients at risk may include knee replacements, hip replacements, pelvic inflammatory disease, pelvic surgeries, radiation, and even simply obesity.
Once the blockage or narrowing in the vein is identified in the lab, a balloon is first placed within the blockage to stretch the narrowing, and then a stent is inserted. The stent acts as a spring to keep the vein open. Following the procedure, and anticoagulant is usually prescribed. This allows time for the vein to grow over the stent and avoid clotting within the stent.
Before the Procedure
Follow any instructions you are given on how to prepare, including:
- Do not eat or drink anything for 6 hours before the procedure.
- Tell your radiologist what medications, herbs, or supplements you take; if you are, or may be, pregnant; or if you are allergic to contrast medium (x-ray dye) or other medications.
During the Procedure
- You’ll change into a hospital gown and lie on an x-ray table. An IV (intravenous) line is started to give you fluids and medications. You may be given medication to help you relax. The skin at the insertion site is numbed with medication.
- A very small incision is made over the insertion site. Then, a needle with a thin guide wire is inserted through the skin into the vein. A catheter (thin, flexible tube) is placed over the guide wire into the blood vessel.
- Contrast medium is injected into the blood vessel. This helps the veins show clearly on x-ray images. Using these images as a guide, the radiologist moves the catheter to the narrowed or blocked part of the vein. Before and after a procedure an intravenous ultrasound maybe performed to show the how much the vein has been widened.
- When the catheter reaches the narrowed or blocked area, a special balloon attached to the catheter is inflated (angioplasty). This widened the passage through the vein.
- To hold the vein open, a stent may then be inserted. To do this, a catheter with a stent attached is threaded over the guide wire. When the stent reaches the narrowed area, it is opened fully. The stent stays in the artery and the catheters and balloons are removed.
- When the procedure is done, the catheter, wire, and balloons are removed. The stent remains in place.
Potential Risks and Complications
- Bruising at the catheter insertion site
- Damage to the vein, including worsening of blockage
- Problems due to contrast medium, including allergic reaction or kidney damage
- Restenosis (reblockage) of the artery, often within 6 to 18 month
After the Procedure
- You may stay in the hospital for a few hours or overnight.
- Drink plenty of fluids to help flush the contrast medium from your system.
- Care for the insertion site as directed.
Venous Stenting Importance Explained by Dr. Jamnadas
“This patient started experiencing significant bilateral lower extremity swelling, and although the differential diagnosis includes congestive heart failure, pulmonary hypertension, lung disease, liver disease, we have seen many patients who have iliac vein stenosis. This is the large vein that drains the lower extremities, and when there is a narrowing in these veins, one gets venous hypertension in the lower extremities which results in swelling, skin discoloration, even ulcerations which take a very long time to heal, leg heaviness, varicose veins, and unless the diagnosis is accurately made, the patients end up getting unnecessary diuretics, or progression of venous disease in the lower extremities.
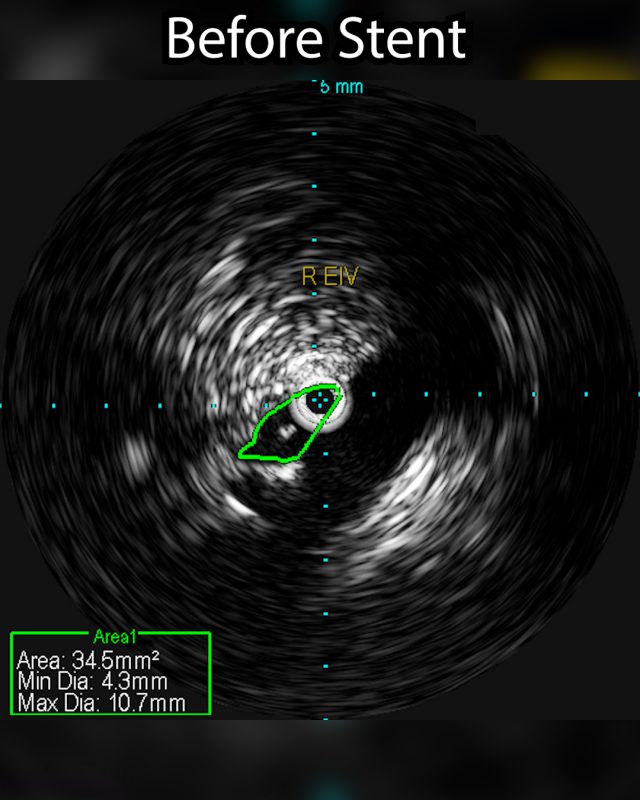
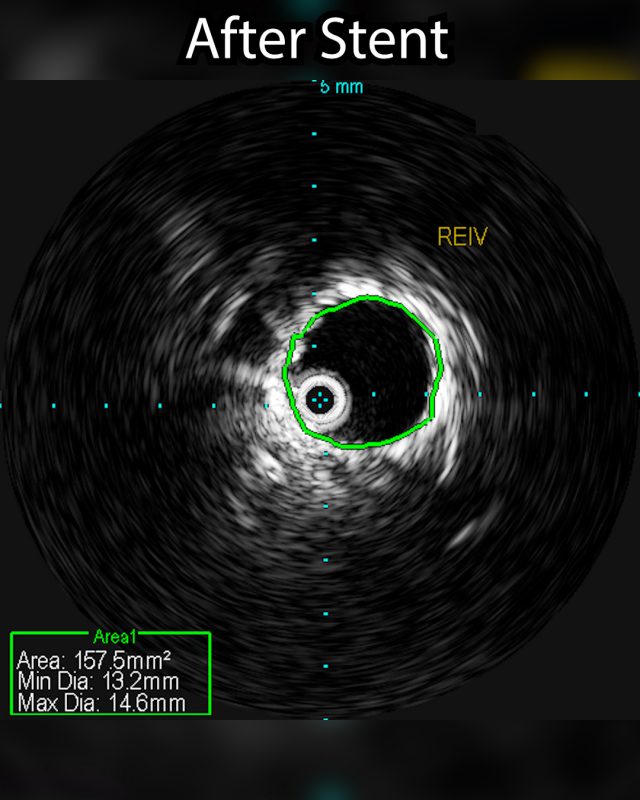
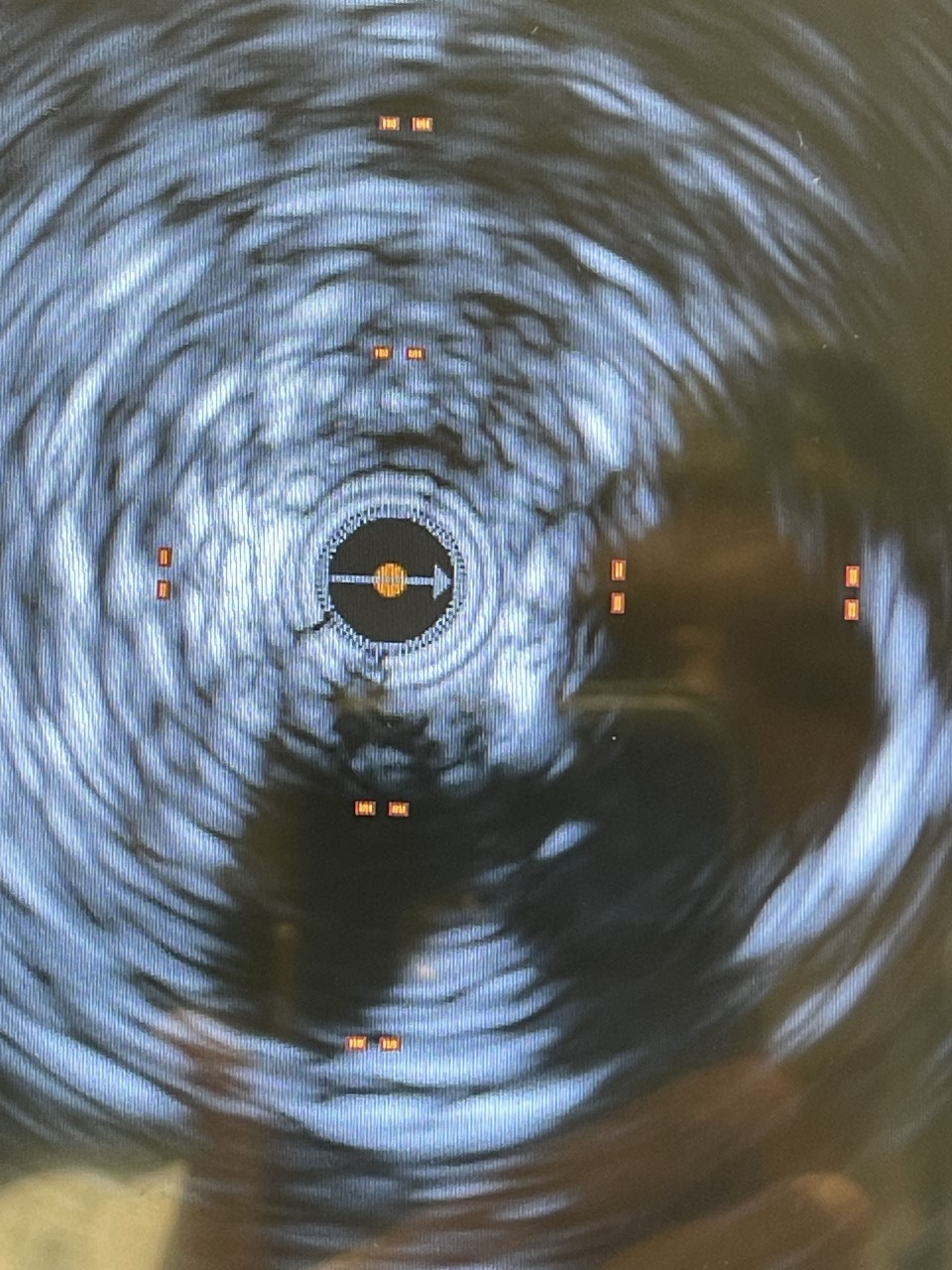
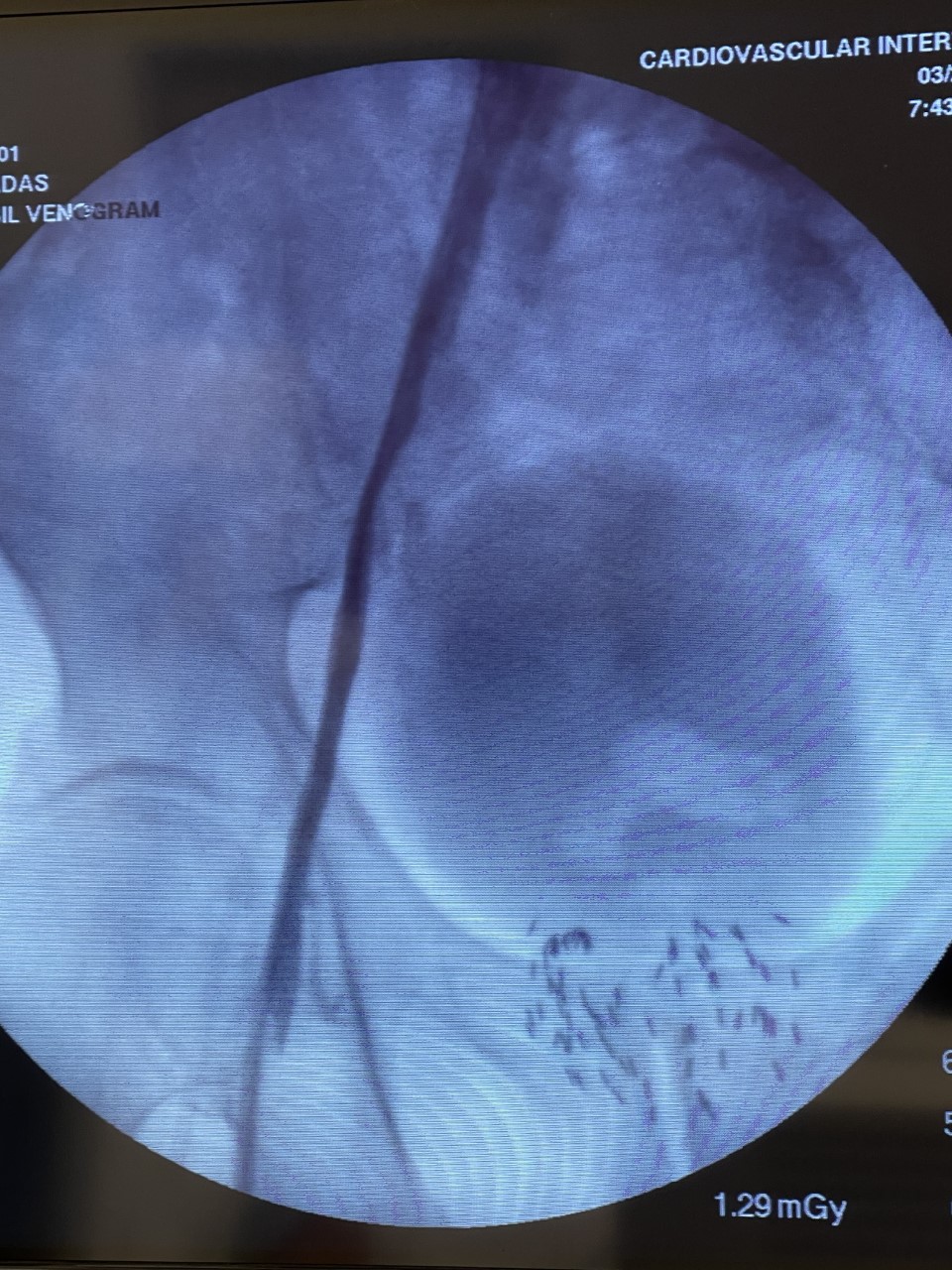
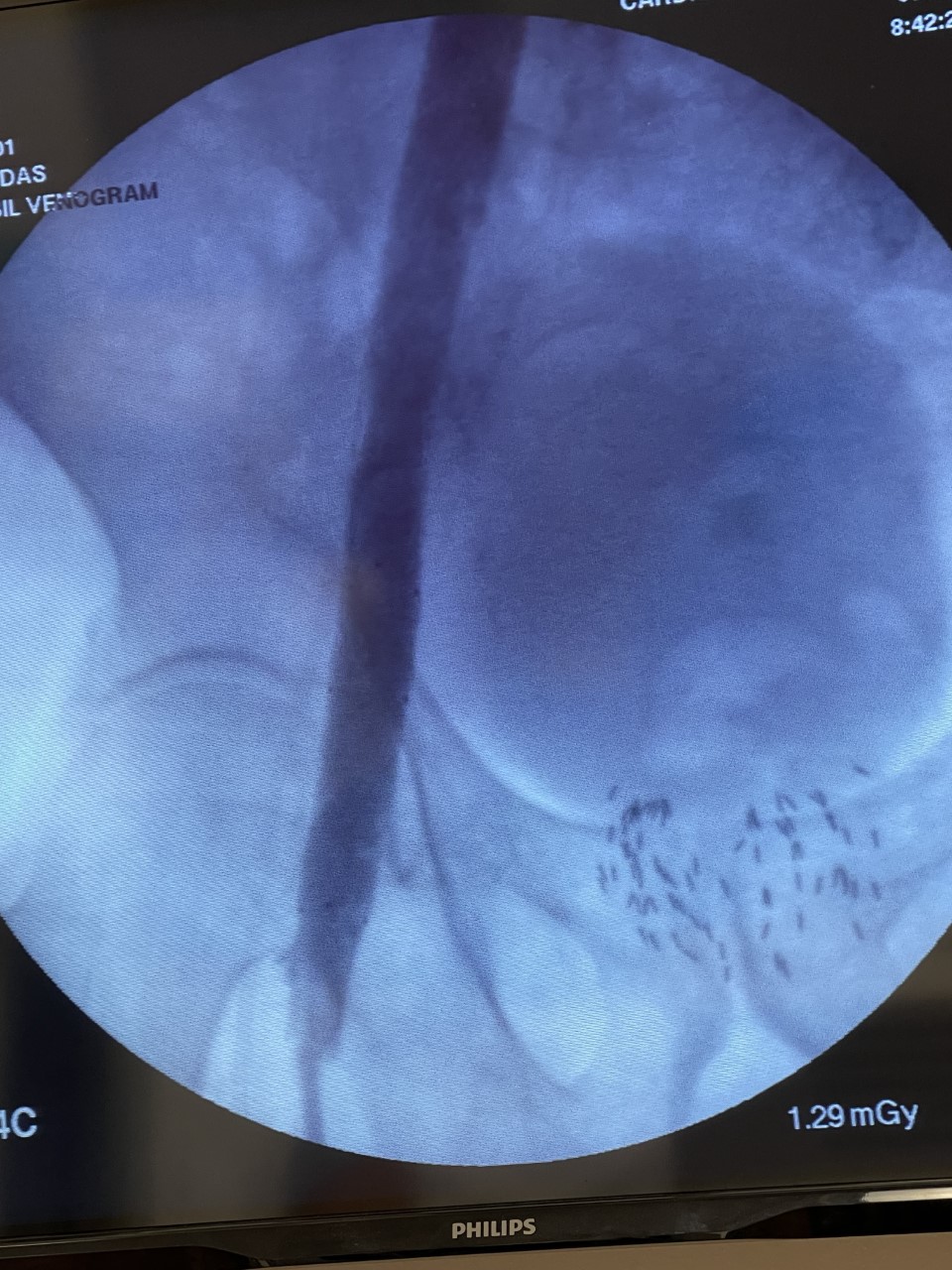
The venogram underestimates the percentage stenosis and therefore the intravascular ultrasound is needed. This involves placing a wire into the iliac vein from the femoral vein, and then examining the inside of the vein using the ultrasound as demonstrated in the 1st photograph. This demonstrated critical stenosis of the veins and then, a stent placement was done. A stent is a self expanding spring like structure placed within the vein, expanding its lumen, and thereby decompressing the lower extremities allowing the blood to drain out of the leg, and then the lower extremity swelling improves.
This is a grossly under recognized cause of lower extremity venous problems. Iliac venous stenosis mostly goes unrecognized. The patient’s that may have this condition also include patients who have had blood clots in the lower extremities before, extensive trauma to the lower extremities, extensive knee surgeries or hip surgeries, pelvic surgery, because all these do predispose to sluggish flow stagnation within the iliac veins irritation of the vein, fibrosis, and then finally narrowing. Blood clots can sit in the iliac veins and become endothelial lysed resulting in fibrosis and calcification of the veins as well. Many patients have no active clots left in the lower extremities, but still have swelling in the lower extremities and it is because of venous hypertension caused by pelvic disease from blood clots that are narrowing the iliac veins.”