What is Peripheral Angioplasty?
An Illustration of a blockage before and after stent placement
Angioplasty is an invasive procedure used to widen a narrowed or blocked artery using a thin catheter with a balloon at the end.
A blocked artery can occur anywhere in the body. Blockages are due to the formation of fatty plaques known as atherosclerosis. When this plaque ruptures, a clot will form leading to further obstruction of the artery. When this occurs in the peripheries it is known as peripheral vascular disease. The procedure for this is known as percutanteous transluminal angioplasty (PTCA).
The balloon catheter is positioned in the narrowed segment of the artery. Inflation of the balloon causes the balloon to push outward against the blockages and surrounding wall of the artery allowing blood to flow through more easily.
A metal mesh stent may be left in the artery after an angioplasty is done.
As plaque builds up in the arteries, it becomes more difficult for blood to reach the body’s tissues. When the tissues are deprived of the oxygen rich blood it needs, symptoms may occur.
Who needs it?
Peripheral Angioplasty is used to treat symptoms caused by:
- Peripheral Vascular Disease: symptoms of claudication, pain or cramping in the legs, or cold feet.
- Carotid Artery Disease (narrowing of artery in the neck): symptoms of syncope or fainting, dizziness, or blurring of vision.
- Renal Artery Disease (narrowing of arteries in kidney): symptoms of high blood pressure.
Why do I need it?
Angioplasty is useful in treating blockages in any of the blood vessels when medications or lifestyle changes are not enough to improve blood flow.
Angioplasty can be done to relieve any symptoms you may be having due to the decreased blood flow to the tissues.
How to prepare for the procedure:
You will be asked to have blood work done some time before the procedure.
Do not eat or drink anything from midnight the night before your procedure. You may have small sips of water to take your medicine. The procedure is usually done in the morning.

If taking anticoagulants such as Coumadin, you may be asked to stop 5 days before the procedure.
If you are diabetic and taking oral medications, you may be asked not to take it the morning of your procedure. If you are taking insulin, you may be asked to take half the dose you normally take.
Avoid using any medications used for erectile dysfunction including Viagra, Cialis, and Levitra) 4 days before the procedure.
Check with Dr. Jamnadas several days before the procedure to determine which medications you may need to stop.
The possible risks and benefits will be explained to you and any questions you or your family may have will be answered before your procedure.
Remove nail polish, necklaces, rings, bracelets, and any other jewelry before the test.
You will be admitted into the hospital so be prepared with an overnight bag.
Make arrangements to have someone drive you to and from the hospital. You will not be permitted to drive after the procedure.
Bring a list of the names and dosages of all the medications you are on.
Let us know if you have had any previous allergic reactions to a contrast dye, iodine, or history of bleeding problems.
You will be asked to empty your bladder before the procedure.
During the Procedure:
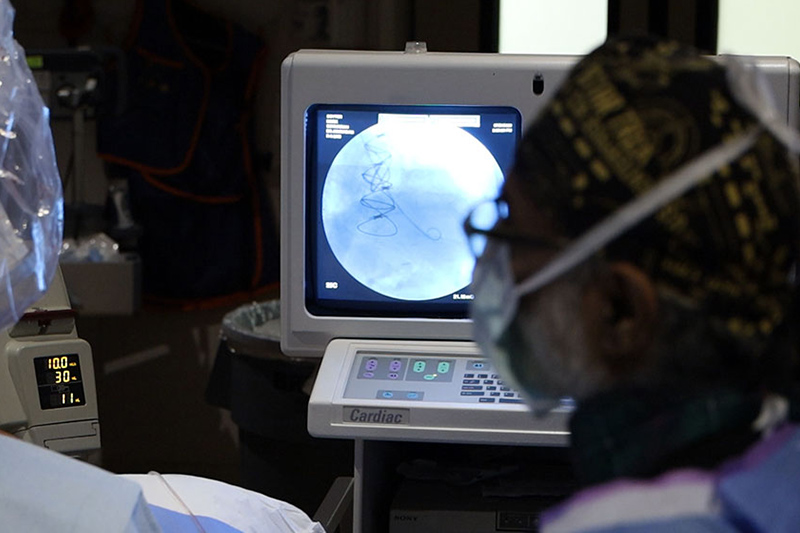
The procedure will be carried out at the hospital in the Cardiac Catheterization Laboratory (Cath Lab).
During the procedure you will lay awake on a table on your back.
Several electrodes will be attached to your arms, legs, and chest. These electrodes have leads that will connect to an electrocardiogram (EKG) machine that records the electrical activity of the heart throughout the test.
An I.V. will be inserted into your arm or hand. From this I.V. a sedative will be given to you to help you relax.
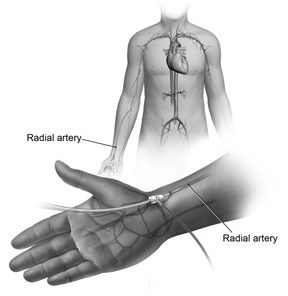
Under sterile precautions, Dr. Jamnadas will inject a local anesthetic until you are fully numb in the area where the catheter will be inserted. The catheter can be inserted either into the radial (wrist), brachial (inside your elbow), carotid (neck), or most commonly the femoral (groin) artery.
The radial approach may be better suited for you rather than the femoral approach for the following reasons:
- Limited bed rest after the procedure, usually only 15 minutes. It is easy on patients with back problems or patients who can not lie down for a long period of time.
- Does not require pressure on the groin.
- Less bleeding risks.
- Do not need to stop anticoagulants before the procedure.
A small incision is made in the skin, and a needle is used to enter the artery. A guide wire is threaded into the artery. A short plastic tube known as a sheath is slipped over the guide wire and into the artery.
The guide wire is then removed. Once the sheath is in place, the catheter can be inserted.
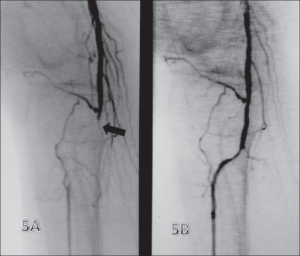
A contrast dye will be given to view the arteries and seen under x-ray guidance. This allows Dr. Jamnadas to see the exact number, location, and size of the blockage.
Once the blockage is located, the catheter is advanced through the artery to the narrowed segment. A balloon is then inflated, compressing the plaque against the artery wall.
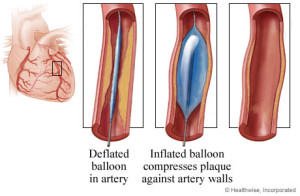
Restenosis is the recurrence of stenosis, a narrowing of a blood vessel, leading to restricted blood flow. Since the restenosis (re-narrowing) rate is high in angioplasty, a stent is often placed which acts as a scaffolding to keep an artery open to ensure blood flow.
After the Procedure:
Once the procedure is done, the puncture site in the artery will be closed.
You need to remain lying down for several hours.
If the insertion site was in the groin, the introducer sheath is usually removed within 6 hours of the procedure. You may need to lie down for 2-6 hours without bending or lifting your leg.
If the catheter was inserted into your wrist or arm, you will be permitted to get out of bed sooner.
After this you will be allowed to move about freely. This does not allow strenuous activity up to 1–2 days.
A nurse will monitor your heart rate, blood pressure, temperature, and the insertion site.
You will be asked to drink plenty of fluids after the procedure to flush out the contrast dye from your system.
It is normal to have a small bruise or lump at the insertion site. This should disappear in about 2 weeks.
What are the risks?
Angioplasty is a common interventional procedure, although with any medical procedure it carries risks. Most of the complications, if they occur are minor and temporary.
These include:
- Allergic reaction: may have an allergic reaction to the contrast dye.
- Nausea and Vomiting
- Bleeding, bruising, or swelling at the insertion site.
- Blockage may reoccur.
- Arrhythmia: irregular heart rhythm
- Infection
- Damage to the heart or blood vessels
- Kidney damage: due to the contrast material which could possibly cause kidney failure.
- Heart attack or stroke: on rare occasion, the catheter may dislodge a clot or debris from the inside wall of the artery.
What are the benefits?
-
Angioplasty can restore blood flow in the artery without requiring a major surgery.
- Does not require an incision.
- General anesthesia is not required.
- Recovery time is short.
- Can be done within an hour of an emergency situation such as heart attack to reverse damage.
- You may feel better than you have felt in a long time.
What is the disadvantage?
A disadvantage of angioplasty is that there is a high restenosis rate.
The artery re-narrows over time caused by the growth of new tissue at the site where the artery was widened or may block again.
This can be prevented by inserting a stent.