What is Cardiac Catheterization?
A catheterization, also called an “angiogram,” is an invasive procedure that allows Dr. Jamnadas to evaluate the hearts function.
A cardiac catheterization is used to determine the presence of heart structural defects, coronary artery disease, valvular disease, or disease of the aorta. This can show whether further cardiac treatment is needed.
Who needs it?
Cardiac catheterization is done in patients with:
1. Symptoms of Coronary Artery Disease (plaque build up in the cardiac blood vessels) including:
-
- Angina- chest pain or discomfort which usually occurs on exertion or stress.
-
- Dizziness
-
- Heart attack- occurs when a coronary artery becomes completely blocked.
-
- Heart failure – heart fails to pump adequately.
-
- Abnormal Nuclear Stress Test
-
- Abnormal Coronary CT Angiogram
2. Heart Valve Disorders
-
- Valvular Stenosis- narrowing of a heart valve, preventing it to open completely.
-
- Valvular Regurgitation- known as a ‘leaky’ valve, preventing the complete closure of the valve.
3. Congenital Heart Defects- deformity in the heart starting from birth.
4. Cardiomyopathy- weakening of the muscles of the heart leading to the dilatation and enlargement of chambers within the heart.
Why do I need it?
A cardiac catheterization provides accurate and detailed information of how well your blood is flowing to the heart. This allows Dr. Jamnadas to diagnose a problem accurately and also allows him to choose the best treatment for you.
Catheterization is usually done to:
- Evaluate or confirm coronary heart disease, valvular or aortic disease.
- Evaluate heart muscle function
- Determine whether further interventional procedure is necessary.
- Determine how well blood flow is after interventional procedure is done.
How to prepare for the procedure
You will be asked to have blood work done some time before the procedure.
Do not eat or drink anything from midnight the night before your procedure. You may have small sips of water to take your medicine. The procedure is usually done in the morning.
If taking anticoagulants such as Coumadin, you may be asked to stop 5 days before the procedure. Please see your instructions
If you are diabetic and taking oral medications, you may be asked not to take it the morning of your procedure. If you are taking insulin, you may be asked to take half the dose you normally take.
Avoid using any medications used for erectile dysfunction including Viagra, Cialis, and Levitra) 4 days before the procedure.
Check with Dr. Jamnadas several days before the procedure to determine which medications you may need to stop.
The possible risks and benefits will be explained to you and any questions you or your family may have will be answered before your procedure.
Remove nail polish, necklaces, rings, bracelets, and any other jewelry before the test.
Make arrangements to have someone drive you to and from the hospital. You will not be permitted to drive after the procedure.
Be prepared with an overnight bag. If interventional procedure is needed during the diagnostic catheterization, you will be required to stay overnight.
Bring a list of the names and dosages of all the medications you are on.
Let us know if you have had any previous allergic reactions to a contrast dye, iodine, or history of bleeding problems.
You will be asked to empty your bladder before the procedure.
During the procedure
The procedure will be carried out in the hospital in the Cardiac Catheterization Laboratory (Cath Lab).
During the procedure you will lay awake on a table on your back.
Several electrodes will be attached to your arms, legs, and chest. These electrodes have leads that will connect to an electrocardiogram (EKG) machine that records the electrical activity of the heart throughout the test.
An I.V. will be inserted into your arm or hand. From this I.V. a sedative will be given to you to help you relax.
Under sterile precautions, Dr. Jamnadas will inject a local anesthetic until you are fully numb in the area where the catheter will be inserted. The catheter can be inserted either into the radial (wrist), brachial (inside your elbow), carotid (neck), or the femoral (groin) artery.
The radial approach may be better suited for you rather than the femoral approach for the
following reasons:
- Limited bed rest after the procedure, usually only 15 minutes. It is easy on patients with back problems or patients who can not lie down for a long period of time.
- Does not require pressure on the groin.
- Less bleeding risks.
- Do not need to stop anticoagulants before the procedure.
A small incision is made in the skin, and a needle is used to enter the artery. A guide wire is threaded into the artery. A short plastic tube known as a sheath is slipped over the guide wire and into the artery. The guide wire is then removed. Once the sheath is in place, the catheter can be inserted.
A contrast dye will be given to view the arteries and seen under x-ray guidance. This allows Dr. Jamnadas to see any abnormalities in the arteries including blockages.
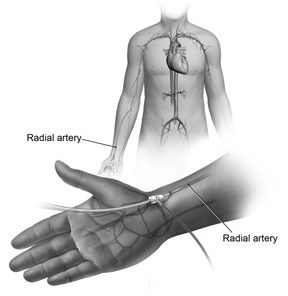
Transradial cardiac catheterization is a procedure used to treat and diagnose certain heart conditions. Taking a Radial approach is less invasive for the patient.
In the event that a severe narrowing or blockage is identified, Dr. Jamnadas will proceed with an interventional procedure are such as angioplasty and stenting.
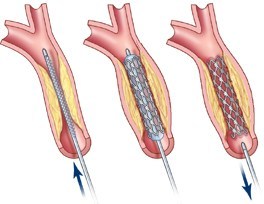
A stent is a tiny tube that your doctor can insert into a blocked passageway to keep it open.
Angioplasty is when a wire with a deflated balloon is passed through the catheter to the narrow area. The balloon is then inflated, compressing the plaque against the artery wall and widening it, so it no longer restricts blood flow.
A stent may be placed that acts as a scaffolding to keep an artery open and ensure blood flow and prevent re-narrowing.
After the procedure
Once the procedure is done, the puncture site in the artery will be closed.
You need to remain lying down for several hours.
If the insertion site was in the groin, the introducer sheath is usually removed within 6 hours of the procedure. You may need to lie down for 2-6 hours without bending or lifting your leg.
If the catheter was inserted into your wrist or arm, you will be permitted to get out of bed sooner.
After this you will be allowed to move about freely. This does not allow strenuous activity up to 1–2 days.
A nurse will monitor your heart rate, blood pressure, temperature, and the insertion site.
You will be asked to drink plenty of fluids after the procedure to flush out the contrast dye from your system.
It is normal to have a small bruise or lump at the insertion site. This should disappear in about 2 weeks.
Depending on the outcome of the procedure, you may be sent home about 6 hours after the procedure or may have to stay overnight in the hospital.
What are the risks?
Most of the complications if they occur, are minor and temporary.
These include:
- Allergic reaction: may have an allergic reaction to the contrast dye.
- Nausea and Vomiting
- Bleeding, bruising, or swelling at the insertion site.
- Arrhythmia: irregular heart rhythm
- Infection
- Damage to the heart or blood vessels
- Kidney damage: due to the contrast material which could possibly cause kidney failure.
- Heart attack or stroke: on rare occasion, the catheter may dislodge a clot or debris from the inside wall of the artery.