What is Peripheral Vascular Disease?
Peripheral vascular disease is a disease of the arteries of the circulatory system due to atherosclerosis. Atherosclerosis is a gradual build-up of fat in the arterial walls depriving the limbs of the oxygenated blood flow it needs.
Atherosclerosis is not confined to one artery but may involve other areas as well.
Most commonly peripheral vascular disease is seen in the legs and is noticed by intermittent pain while walking.
Similarly, when atherosclerosis affects the heart it is called coronary artery disease.
What causes peripheral vascular disease?
- Congenital: some individuals develop structural defects in the blood vessels at birth.
- Autoimmune: people with autoimmune conditions can develop inflammation of the blood vessels known as vasculitis.
- Thrombosis: a blood clot can narrow or obstruct a blood vessel.
- Diabetes: can cause damage to the blood vessels which can make them more likely to be weakened or narrowed.
- Infective: certain infections like syphilis can cause inflammation and scarring leaving a blood vessel weak or narrow.
- Trauma
What are the risk factors?
- Genetic: Inherited tendency within the family
- Age: increasing age, above 50 years
- Sex: Men are slightly more at risk than women
- Family history of peripheral vascular disease, heart disease, or stroke
- Smoking
- Diabetes
- Obesity (BMI > 30)
- High blood pressure
- High cholesterol
- Sedentary lifestyle
- Coronary artery disease
- High levels of homocysteine
What are the symptoms?
- Pain or cramping in the hip or thigh during walking or climbing up stairs
- Tingling or numbness in the legs
- Feet that feel cold
- Slow healing of cuts or sores on the feet and legs
- Pale, shiny, or bluish skin
- Brittle and slow growing nails
- Loss of hair over the limbs
- Absent or weak pulse in the legs or feet
- Erectile dysfunction
What are the complications?
- Permanent tingling, numbness, or weakness in the legs or feet
- Permanent burning or aching pain which can lead to an excruciating pain
- Leg or foot ulcers
- Gangrene – death of a part of the body due to lack of blood supply. Treatment will be amputation of the affected part.
- Stroke and heart attack- people with peripheral vascular disease are at higher risk of heart attack and stroke
- Renal artery disease or stenosis- blocking the blood flow to the kidneys.
How is it diagnosed?
- Discussing with you about your symptoms, risk factors, medical and family history.
- On physical examination– weak or absent peripheral pulses along with other signs of peripheral vascular disease will be looked for.
- Blood tests– measuring your lipid profile and glucose levels in case diabetic.
By performing tests including:
- Ankle Brachial Index (ABI) – this is a non-invasive test measuring the ratio of blood pressure in the ankle to your arm. If the value is lower than expected, this may indicate a vascular problem. You may be required to walk on a treadmill and have readings taken before and after exercise.
- Ultrasound Doppler Test– helps to evaluate the blood flow through a vessel and identify the site of blocked or narrowed arteries.
- Angiogram– allows Dr. Jamnadas to locate the exact anatomical site of blockage by injecting a dye within the arteries, which is visualized on x-ray showing the amount of blood flow to an area, and the number, size, and location of any blockages.
How is it treated?
- Quit smoking!!
- Limit alcohol intake if you chose to drink
- Lower blood sugar levels
- Maintain a normal blood pressure and cholesterol
- Eat a well-balanced diet
- Eat foods high in fiber such as whole grain cereals, oatmeal, and figs. Eat plenty of fruits such as apples, bananas, prunes, oranges, and pears. Include fish and legumes such as beans or chickpeas.
- Lower your salt intake
- Avoid fatty foods including bad saturated fat that is found in some meats, dairy products, chocolates, baked goods, and deep-fried food.
- Exercise regularly for 30 minutes at least 3-4 times a week and be more physically active
- Maintain a healthy weight with a BMI below 25
- If you have diabetes, practice proper foot care and prevent injury to the foot. Avoid walking barefoot and wear proper shoes. Maintain toenails and skin care. Be sure to inspect the soles of your feet regularly.
- Cholesterol-lowering medications– these act by decreasing the amount of cholesterol in blood, especially Lowering your low-density lipoprotein (LDL- your Lousy cholesterol) and keep your high-density lipoprotein (HDL- your Healthy cholesterol) High
- High blood pressure medications– such as Beta blockers that slow your heart rate and reduce blood pressure which decreases the oxygen demand of the heart
- Antiplatelet medication– such as aspirin or Plavix which prevents platelets clumping together. This thins the blood and reduces the chances of a blood clot narrowing or obstructing the arteries. This is not appropriate for all patients including patients with bleeding disorders or already taking a blood thinner.
- Controlling of blood sugar
- Cilostazol (Pletal) – used for claudication and pain relief by increasing the blood supply to the limbs by dilating blood vessels and preventing clots.
- Pentoxifylline (Trental) – this is an alternative medication which is less effective than Cilostazol but has fewer side effects of headache and diarrhea.
- Fish and Fish Oil- are high in omega 3 fatty acids, especially in fish like salmon, herring, and tuna. Fish oil supplements are also high in omega 3 fatty acids.
- Flax and flaxseed oil- contain omega 3 fatty acids and fiber
- Greensoul- is a natural supplement that helps to maintain a healthy cholesterol level, supports the body’s immunity, and the ability to fight free radicals.
- Coenzyme Q10- helps maintain a healthy cholesterol level, boosts immunity, and energy.
- Perfusion SR- helps enhance blood flow, maintain a normal blood pressure, and enhance the elasticity of large arteries.
- Angioplasty and stent placement: this is a procedure considered as non-surgical because it is done by Dr. Jamnadas, who accesses the artery by inserting a long, thin tube (catheter) into the narrowed part of your artery while being visualized under x-ray. A wire with a deflated balloon is passed through the catheter to the narrow area. The balloon is then inflated, compressing the plaque against the artery wall and widening it, so it no longer restricts blood flow.
- Atherectomy: is a procedure where a catheter is used to scrape the inner lining of an artery. That material which is blocking the artery is extracted and then taken out of the artery using the catheter. The procedure is Best suited for blocked arteries in the legs. Laser Arthrectomy has been used in the legs also, but Dr. Jamnadas does not favor it at this time due to the high re-stenosis rate.
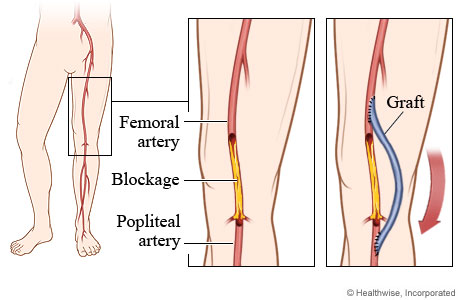
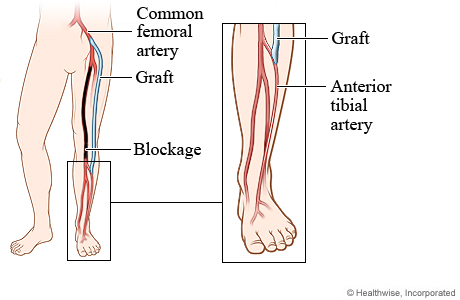
- Bypass Surgery: is performed by removing a portion of a small blood vessel and sewing or ‘grafting’ one end of the bypass proximal to the area of blockage and the other end beyond the area of blockage, therefore bypassing the affected area.
If your disease is very severe and these procedures are not recommended for you, your foot or leg may need to be removed (amputated). This is usually necessary if you have very little to no blood flow leading to death of the tissues which can cause risk of a life-threatening infection.
Amputation is a last resort, but if peripheral vascular disease is not controlled, it is a possible result.
How can I prevent this?
- Do not smoke!
- Maintain a healthy weight with a BMI <25
- Maintain a normal blood pressure, cholesterol and sugar levels
- Eat nutritious, low fat foods and avoid foods high in cholesterol
- Exercise regularly for 30 minutes at least 3-4 times a week