What is Hyperlipidemia?
Hyperlipidemia refers to elevated levels of lipids (fats) in blood. These lipids include cholesterol and triglycerides. Elevated levels of lipids can significantly increase your risk of heart disease.
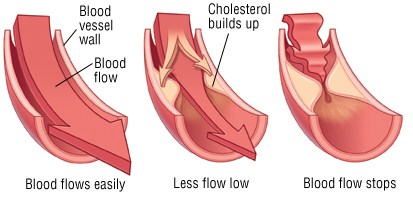
Elevated lipids in blood deposit into the walls of blood vessels and form plaque. Constant elevation of these levels can increase the deposits laid in the vessel walls. These plaques restrict the blood flowing through the vessels depriving tissues of the oxygen and nutrients it needs. This plaque has a potential of rupturing. Once the plaque ruptures, a clot will form and further narrow the blood flow to tissues.
This narrowing of the arteries is called atherosclerosis. When atherosclerosis affects the heart it is called coronary artery disease. This causes symptoms of chest pain and can lead to a heart attack. Atherosclerosis of the peripheries is known as peripheral vascular disease which causes symptoms of leg pain while walking called claudication. Atherosclerosis can even narrow the vessels supplying the brain causing dizziness. A clot may dislodge and block a vessel in the brain causing stroke.
Hyperlipidemia can significantly increase a person’s risk of heart attack and stroke!
What causes this?
-
Genetic- hyperlipidemia runs in the family due to a genetic mutation.
- High saturated fatty diet
- Obesity
- Sedentary lifestyle- lack of physical activity
- Endocrine disease- Diabetes, hypothyroidism, and adrenal disease
- Kidney disease
- Liver disease
What are the different types of lipids?
Lipids are made up of cholesterol and triglycerides. Lipids are transported in blood as parts of larger complexes known as lipoproteins.
Blood tests measure the level of your lipoproteins. This blood test is performed here in our clinic with same day results. The measurement of these lipids is known as your lipid profile.
The standard lipid profile measures:
- Total Cholesterol
- Low Density Lipoprotein (LDL)
- High Density Lipoprotein (HDL)
- Triglycerides
-
Total Cholesterol- this measures all the overall cholesterol components in blood.
This level includes your good and bad cholesterol; therefore this is not an indicator to start medications.
Total cholesterol levels can be checked at any time of the day and does not require fasting.
Normal levels: Below 200 mg/dl
- Low Density Lipoprotein (LDL) – this is sometimes referred to as your Lousy cholesterol. LDL cholesterol builds up in the arteries making them narrow. Your LDL is the most accurate component for checking the risk of heart disease.
An accurate LDL level is achieved after a 12 hour fast.
Optimal levels: Below 70mg/dl in high risk patients; below 100mg/dl intermediate risks; below 120mg/dl low risk patients
- High Density Lipoprotein (HDL) – this is sometimes referred to as your Healthy cholesterol. HDL picks up excess cholesterol and takes it back to the liver instead of it accumulating in the arteries. – That’s a good thing!
Like total cholesterol, HDL can be checked at any time of the day without fasting.
Normal levels: Above 60mg/dl
- Triglycerides- this is found in a type of lipoprotein called very low density lipoprotein. Triglycerides accumulate in the arteries and can be atherogenic.
Triglycerides should be checked with a 12 hour fast for accurate levels.
Normal levels: Below 150mg/dl
Who is at risk?
Positive Risk Factors Negative Risk Factors
Family history of heart disease High HDL levels
Increasing age
Low HDL levels
Smoking
High Blood Pressure (Hypertension)
Obesity
Poor Diet
Diabetes
Lack of exercise
When should I get my lipid profile done?
Screening should be started at the age of 35 in patients with no risk factors
With risk factors, screening should be started at the age of 20-25.
You must have your lipid profile checked at least once by the age of 45.
Depending on your risk factors and lipid levels, you may be screened every 5 years or more frequently, if risk factors are present.
How is it treated?
Lifestyle changes:
The first line of treatment is lifestyle changes. Lifestyle changes not only treat, but prevent hyperlipidemia.
A few ways you can modify your lifestyle are by:
Quit smoking if you are a smoker.
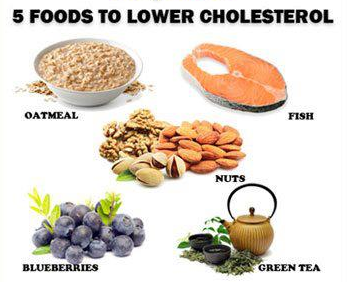
Reduce the amount of saturated fats and cholesterol you take. Saturated fats include cheese, butter, milk, and red meats.
Add more fruits and vegetables to your diet.
Try eating fish like cod, salmon, or tuna. These are low in fat and have healthy omega 3 fatty acids.
Increase fiber in your diet. This helps in lowering cholesterol levels. Eat more whole grain foods like brown rice and oatmeal.
Reduce your weight. Maintain a BMI below 25.
Exercise for 30 minutes at least 3-4 times a week and be more physically active.
Medications:
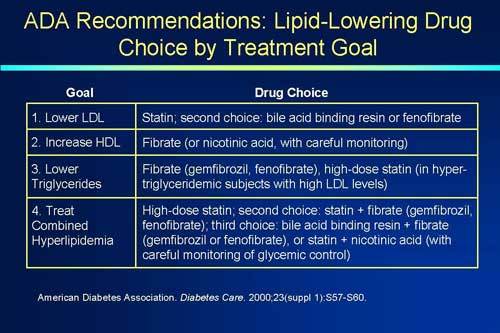
Medications are to be used along with lifestyle changes.
Dr. Jamnadas or Dr. Kelly will chose a medication or combination of medications depending on age, risk factors, your present health, and possible side effects of the drug.
After initial therapy, your lipid profile will be monitored at 6 week intervals until target levels are reached. Monitoring will then be done every 6-12 months.
Lipid lowering medications include:
-
Statins- statins are extremely useful in lowering your lousy LDL by 25- 60%. They are also used in the prevention of heart disease. Statins act by blocking a step in cholesterol synthesis in the liver and enhances the clearance of LDL from circulation.
Statins include: Simvastatin (Zocor), Atorvastatin (Lipitor), Lovastatin (Altoprev, Mevacor), Pravastatin (Pravachol), Rosuvastatin (Crestor), and Fluvastatin (Lescol).
- Bile acid sequestrants- these agents block the absorption of bile acids from the gut that the liver uses to make cholesterol. These help in lowering only mild to moderately elevated LDL and slightly increase HDL.
These may interfere with fat soluble vitamin absorption including vitamins A, D, K, and E. The effects of this can be minimized by taking the drug at different times of the day.
Bile acid sequestrants include: Cholestyramine (Prevalite, Questran), Colestipol (Colestid), and Colesevelam (WelChol).
- Ezetimibe (Zetia) – this blocks the absorption of cholesterol from the food in your diet.
- Ezetimibe-Simvastatin (Vytorin) – this is a combination of a statin and ezetimibe. This lowers the absorption of cholesterol from your diet and lowers the synthesis of cholesterol from the liver.
- Niacin (Niaspan) – is a vitamin that decreases triglyceride levels by limiting the synthesis of LDL and VLDL, and increases HDL.
- Fibrates– these lower the synthesis of LDL moderately and increase HDL by 10-15%.
Fibrates include: Gemfibrozil (Lopid) and Fenofibrate (Tricor, Triglide).
Alirocumab (Praluent) – Lowers LDL by increasing cholesterol removal by the liver
Supplements:
Food and supplements rich in omega 3 fatty acids help reduce triglyceride levels and lower the risk of heart disease.
-
Fish and Fish Oil: are high in omega 3 fatty acids, especially in fish like salmon, herring, and tuna. Fish oil supplements are also high in omega 3 fatty acids.
- Flax and flaxseed oil: contain omega 3 fatty acids and fiber.
- Greensoul: is a natural supplement that helps to maintain a healthy cholesterol level, supports the body’s immunity, and the ability to fight free radicals.
- Coenzyme Q10: helps maintain a healthy cholesterol level, boosts immunity, and energy.
What are the complications?
High lipid levels can lead to atherosclerosis. Atherosclerosis can affect any artery in the body and may lead to complications including:
-
Coronary artery disease: can lead to chest pain due to narrowing of the arteries in the heart
- Heart attack: the complete obstruction of an artery in the heart due to rupture of plaque and clot formation.
- Peripheral vascular disease: narrowing of the arteries in the legs can lead to leg pain while walking called claudication.
- Stroke: the complete obstruction of an artery in the brain due to a dislodged clot from a ruptured plaque.
How can this be prevented?

The combination of smoking and having high cholesterol dramatically increases your risk of heart attack.
Healthy lifestyle changes can lower your chances of having hyperlipidemia. Set goals for yourself and stick to it. Some ways you can help prevent having high lipid levels are:
- Quit Smoking
- Limit alcohol to a maximum of one glass a day if you chose to drink.
- Eat a low-fat diet with plenty of whole grain foods, fruits, and vegetables
- Lose excess weight! Maintain a BMI below 25.
- Exercise for 30 minutes at least 3-4 times a week and be more physically active.