What is Atrial Flutter?
Atrial flutter is a relatively common abnormal heart rhythm where the atria beat quickly, but evenly. This is similar to atrial fibrillation, but the atria beat quickly and unevenly.
Atrial flutter and fibrillation always have some degree of atrial-ventricular (AV) block with a 2:1 pattern meaning the rate of the ventricles is usually 150 beats per minute while the atria beat at 300 beats per minute. In other words, every other atrial beat reaches the ventricle.
Both of these arrhythmias impair blood flow out of the heart (cardiac output) and promote clot (thrombus) formation.
Animation of Atrial Flutter
How does atrial flutter occur?
Sometimes the electrical impulses ‘short circuit’ and travel across the heart in an abnormal way. Abnormal electrical pathways produce irregular heartbeats and rhythms known as arrhythmias.
Arrhythmias occur when other areas of the heart, other than the SA node, begin sending out their own impulses and take over the pacemaker function of the SA node. The sites that take over could be from any area of the atria, AV node, or ventricles.
The rapid fluttering of the atria does not allow the complete filling of the ventricles, that pumps blood out to the entire body. Symptoms of atrial flutter such as lightheadedness or dizziness may be felt.
Also, some amount of blood remains in the chamber that leads to clot formation.
How is it classified?
Atrial flutter is classified into two types:
Type I (Typical) – more common, atrial flutter rate 240-340 beats/minute, circular (clockwise or counterclockwise) re-entry of electrical patterns in the atria
Type II (Atypical) – rare, atrial flutter rate 340-440 beats/minute, different re-entry pathways
Most patients with atrial flutter will have only one of these. Rarely a patient may present with both types, although they can only occur one at a time.
What are the causes?
Atrial flutter can be due to abnormalities or diseases of the heart, or by diseases elsewhere in the body affecting the heart. Atrial flutter may occur after open heart surgery or substance abuse.
Heart abnormalities and diseases include:
- Congenital heart defects (heart defect from birth)
- Coronary artery disease (decreased blood supply to the heart) or atherosclerosis
- High blood pressure
- Heart attack
- Cardiomyopathy and congestive heart failure
- Rheumatic fever and pericarditis (inflammation of the heart)
- Abnormalities of the heart valves, especially mitral stenosis and mitral regurgitation
- Hypertrophy (enlarged heart)
Diseases elsewhere in the body affecting the heart:
- Hyperthyroidism
- Pulmonary embolism (blood clot in lung)
- Chronic obstructive pulmonary disease (COPD) and emphysema
- Sleep apnea
Substance abuse:
- Consuming large amounts of alcohol (binge drinking)
- Cocaine, amphetamines, diet pills, caffeine, or cold medicines
- Carbon monoxide intoxication
Surgery
- First week following open heart surgery
Who is at risk?
- Increasing age
- Men are at more risk of developing atrial flutter than women
- Family history of atrial flutter
- Drinking alcohol or binge drinking
- Atrial flutter is greatest when an underlying heart disease is associated with left atrial enlargement, left ventricular or biventricular failure
- Heart failure patients and COPD patients
- Other chronic conditions including thyroid disorders and sleep apnea
What are the symptoms?
Some patients may be unaware of their heart beating abnormally.
Although characteristic symptoms include:
- Palpitations (pounding sensation in the chest)
- Fluttering sensation in the chest
- Shortness of breath
- Anxiety
- Weakness
- Dizziness, light-headedness
- Fainting
- Confusion
- Fatigue
- Intolerance to exercise
- Nausea
- Nervousness
- Swelling of the legs or abdomen
What are the complications?
The complications of atrial flutter include:
Syncope (fainting)
Heart failure
Thrombus (clot formation)
Stroke
When should I seek medical care?
If you experience symptoms of atrial flutter, call your physician.
If you have already been diagnosed and being treated for atrial flutter, seek medical help at the hospital as soon as possible if you have the following symptoms:
Severe chest pain
Feeling faint or light-headed
Have an actual episode of fainting
How is Atrial Flutter diagnosed?
The diagnosis of atrial flutter will be based on your history, physical examination, and certain tests.
1. Patient history
Most patients will give a history of characteristic symptoms like palpitations, dizziness, fatigue, shortness of breath, etc.
2. Physical Examination
You will be examined for signs of atrial flutter including:
Rapid, irregular, fast pulse
Heart rate of 100-175 (Normal heart rate = 60-100)
Normal to low blood pressure
Varying heart sounds heard over chest
3. Tests
Certain tests can be performed to determine the cause and severity of your condition including:
Blood tests- to check potassium and thyroid hormone levels
Electrocardiogram- this is a very useful and simple test that records the electrical activity of the heart and reveals atrial flutter or atrial fibrillation. Also shows signs of heart attack, conduction abnormalities, hypertrophy, and electrolyte imbalances.
Chest X-ray- a simple test performed in our office showing the size and shape of the heart. Also reveals the presence of fluid in the lungs.
Echocardiogram (ECHO) – a noninvasive test performed in our office to determine the size and function of the heart’s chambers and the structure and function of the heart valves.
24-Hour Holter monitor- records the electrical events of the heart during your normal daily activities. This is useful in detecting evidence of arrhythmias.
Event monitor- If symptoms of arrhythmia are infrequent and do not occur within 24 hours, an event recorder may be ordered for you for up to 30 days.
Stress test- determines how well the heart works during exercise.
How is it treated?
Atrial flutter treatment goals include restoring the heart to normal rhythm, regulating heart rate, preventing blood clot formation, and treating the underlying cause.
This is done by the use of medications and procedures.
Medications
Some medications are used to slow an irregularly fast heart beat. These decrease the heart rate by slowing the conduction of impulses through the AV node.
These drugs include:
Beta Blockers
Calcium channel blockers
Digoxin
Medications are used to reduce the frequency and duration of atrial flutter and prevent future episodes.
These include:
Amidarone
Sotalol
Propafenone
Flecainide
Medications are used to prevent the formation of blood clots.
These drugs include:
Heparin
Warfarin
Dabigatran
Aspirin
Clopidogrel
Procedures
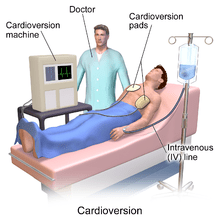
Cardioversion is a medical procedure that restores a normal heart rhythm in people with certain types of abnormal heartbeats (arrhythmias).atrial flutter is sensitive to a low electrical energy direct-current (DC) or medical cardioversion (using an antiarrhythmic drug). DC cardioversion converts atrial flutter into a normal sinus rhythm with high a success rate. Cardioversion may be delayed until starting treatment with an anticoagulant. This medication is usually given for 3-4 weeks, allowing pre-existing clots to resolve. A transesophageal echocardiogram (TEE) is an alternative way of delaying cardioversion, if no blood clots are present, cardioversion may be started. A mild anesthetic is first given, pads are applied over the chest, and then the heart will be shocked into the correct rhythm.
Catheter radiofrequency ablation- is a hospital procedure done to destroy areas on the heart that are causing irregular heart rhythms. A thin flexible tube is inserted into a blood vessel to access the heart. Heat is applied to the tip of the catheter to permanently destroy small areas of abnormal heart tissue. The damaged tissue is no longer capable of generating electrical impulses. A pacemaker may be placed after this procedure
Pacemaker or ICD- a small implantable device used to regulate the heart rate and rhythm. Therefore, the heart contracts in a regular way. An ICD shocks the heart out of the dangerous rhythm.
What is the prognosis?
Atrial flutter can be controlled with treatment.
With treatment, many patients do well.
How can I prevent this?
Atrial flutter can not always be prevented, but there are ways of reducing the risk of developing atrial flutter.
Leading a healthy lifestyle may reduce the chance of coronary artery disease, which can cause atrial flutter.
Some ways you can do this is by:
No smoking!
Be physically active. Engage in moderate physical activity for at least 30 minutes a day
Eat nutritious foods low in cholesterol and fats
Maintain a BMI below 25
Control high blood pressure, cholesterol, and sugar