What is Atherosclerosis?
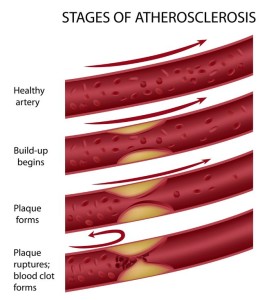
Atherosclerosis is the build-up of fat and cholesterol-filled plaques inside the artery walls, which can restrict blood flow.
These plaques have the potential to rupture leading to the development of a clot. A clot may restrict blood flow further or dislodge and obstruct another vessel.
Atherosclerosis increases the risk of cardiovascular disease including heart attack and stroke.
Atherosclerosis can affect any artery in the body and is a preventable and treatable condition.
How does it occur?
At a young age, fat can start to deposit within the blood vessel walls. Fat builds up over the years can cause injury to the blood vessel walls.
Not only fat, but a number of other substances in blood including inflammatory cells, cellular waste products, proteins, and calcium begin sticking to the inside of vessel wall. All of these substances collectively form what is called Plaque.
Many of the plaque deposits have a soft inner center and hard exterior. If the hard outer surface breaks or tears, the soft inner center will become exposed to our body’s platelets.
The platelets will come to the area of breakage and form a clot around the plaque. This further narrows the artery and restricts blood flow.
A clot may dislodge and permit blood flow again, but the dislodging of a clot can also be dangerous, as it can travel further downstream and cause a blockage.
What are the symptoms?
Animation of the development of atherosclerosis
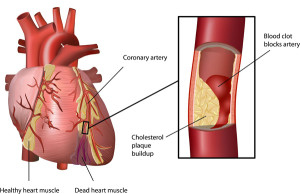
Atherosclerosis can affect any artery in the body. When this condition affects the vessels of the heart it is known as coronary artery disease. Atherosclerosis affecting all other arteries excluding the coronary arteries, it is known as peripheral vascular disease. Atherosclerosis of the vessels that supply the brain can cause as a stroke and may lead to dementia.
Peripheral vascular disease can affect the arteries of the neck, arms, kidneys, legs, etc. Symptoms depend on the part of the body that is affected although; more than one area can be affected.
Coronary artery disease: Symptoms may include chest pain (angina), shortness of breath, dizziness, palpitations, sweating, extreme weakness, fast heartbeat, or nausea.
Peripheral vascular disease:
- Peripheral Vascular Disease: includes symptoms of claudication (pain in the legs while walking), cold feet, tingling or numbness in the legs, slow healing of cuts or sores on the feet and legs, pale, shiny, or bluish skin, brittle and slow growing nails, loss of hair over the limbs, absent or weak pulse in the legs or feet, or erectile dysfunction
- Carotid Artery Disease (narrowing of the artery in the neck): symptoms of syncope or fainting, dizziness, or blurring of vision.
- Renal Artery Disease (narrowing of arteries in kidney): symptoms of high blood pressure.
What are the causes of atherosclerosis?
-
Smoking
-
High blood pressure
-
High cholesterol
-
Diabetes
What are the risk factors?
Non-modifiable risk factors:
-
Age: Old age
-
Sex: Men have a greater risk of atherosclerosis than women. The risk increases in woman after menopause due to less hormone production of estrogen
-
Race: African Americans have more severe high blood pressure than Caucasians. Indians have more diffuse coronary artery disease.
-
Family history of medical diseases associated with cardiovascular disease
Modifiable risk factors:

-
Smoking
-
Excessive alcohol consumption
-
High blood pressure
-
High blood cholesterol levels
-
Uncontrolled diabetes (HbA1c >7.0)
-
Sedentary lifestyle- lack of physical activity is associated with atherosclerosis
-
Obesity
-
Obstructive sleep apnea
-
Chronic inflammation- even having the flu can be a risk because it is a form of inflammation. C-reactive protein is a marker of inflammation and high levels of this can show an increased risk of atherosclerosis.
-
Stress
-
Homocysteine – is an amino acid in the body that helps make protein and maintain tissue. Elevated levels of this can increase the risk of atherosclerosis
-
Fibrinogen- is a protein in the body that aids in blood clotting. An increase in this can increase platelet clumping leading to the formation of clots.
What are the complications?
Complications of atherosclerosis depend on the location of the narrowed or blocked artery.
Coronary artery disease: Complications of coronary artery disease include chest pain (angina), heart attack, congestive heart failure, arrhythmia (abnormal heart rhythm), or pericarditis (inflammation of a layer of the heart).
Peripheral vascular disease:
- Peripheral Vascular Disease: Complications include permanent tingling, numbness, or weakness in the legs or feet, permanent burning or aching pain, leg or foot ulcers, or gangrene (death of a part of the body due to lack of blood supply. Treatment requires amputation of the affected part)
- Carotid Artery Disease: transient ischemic attack (TIA) or stroke
- Renal Artery Disease (narrowing of arteries in kidney): kidney failure
How is it diagnosed?
Your provider / Dr. Jamnadas will have a better idea if you have atherosclerosis by:
- Discussing with you about your symptoms, medical and family history, and risk factors.
- Physical examination- blood pressure will be recorded, peripheral pulses will be felt, and the physician may listen to your arteries for an abnormal whooshing sound called a bruit that may indicate poor blood flow.
- Blood tests- to assess increased levels in cholesterol or elevated blood sugar levels.
- Performing diagnostic tests including:
Electrocardiogram (EKG) – records the electrical activity of the heart. This may show evidence of a current or previous heart attack.
Ankle Brachial Index (ABI) – this is a non-invasive test measuring the ratio of blood pressure in the ankle to your arm. If the value is lower than expected, this may indicate a vascular problem. You may be required to walk on a treadmill and have readings taken before and after exercise.
Ultrasound Doppler Test- helps to evaluate the blood flow through a vessel and identify the site of blocked or narrowed arteries.
Echocardiogram (ECHO) – shows the images of the heart which determines whether the heart walls and pumping activity are normal or performing weakly.
Stress test- helps access the blood flow to the heart at rest and during stress. Will detect if any areas receiving less blood flow.
Chest x-ray- reveals signs of congestive heart failure.
Angiogram- used to locate the exact anatomical site of blockage by injecting a dye into the arteries, which is visualized on x-ray showing the amount of blood flow to an area, and the number, size, and location of any blockages.
Computerized tomography (CT) – helps visualize your arteries. Sometimes an electron-beam computerized tomography (EBCT) is offered to detect calcium within fatty deposits in narrowed arteries.
How is it treated?
The treatment for atherosclerosis may include lifestyle changes, medications, or procedures.
It is very important to reduce any risk factors in order to manage the symptoms and progression of atherosclerosis.
Lifestyle changes
- Quit smoking!!
- Limit alcohol intake if you chose to drink.
- Lower blood sugar levels
- Maintain a normal blood pressure and cholesterol
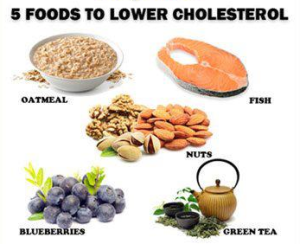
- Eat a well-balanced diet.
- Eat foods high in fiber such as whole grain cereals, oatmeal, and figs. Eat plenty of fruits such as apples, bananas, prunes, oranges, and pears. Include fish and legumes such as beans or chickpeas.
- Lower your salt intake.
- Avoid fatty foods including bad saturated fat that is found in some meats, dairy products, chocolates, baked goods, and deep-fried food.
- Exercise regularly for 30 minutes at least 3-4 times a week and be more physically active.
- Maintain a healthy weight with a BMI below 25.
-
If you have diabetes, practice proper foot care and prevent injury to the foot. Avoid walking barefoot and wear proper shoes. Maintain toenails and skin care. Be sure to inspect the soles of your feet regularly.
-
Relax and reduce stress.
For some people, these changes may be the only treatment needed.
Medications
If lifestyle changes are not enough to control the effects of atherosclerosis, medications may be prescribed to you including:
- Cholesterol-lowering medications– these act by decreasing the amount of cholesterol in the blood, especially Lowering your low-density lipoprotein (LDL- your Lousy cholesterol) and keep your high-density lipoprotein (HDL- your Healthy cholesterol) High.
- Aspirin – is an anticoagulant that prevents platelets from clumping together. This reduces the chances of a blood clot narrowing or obstructing the arteries. This may not be appropriate for all patients including patients with bleeding disorders or already taking an anticoagulant.
- Beta blockers- slow your heart rate and reduce blood pressure which decreases the oxygen demand of the heart.
- Angiotensin-converting enzyme (ACE) inhibitors and Angiotensin receptor blockers (ARBs) – help dilate the blood vessels and lower the blood pressure so the heart does not have to work as hard and improve the lining of arteries. causes positive remodeling of the blood vessels over time.
- Calcium Channel Blockers- medication that helps relax the muscles surrounding the coronary arteries and cause the vessels to open leading to an increase in blood flow to the heart and lowering blood pressure.
Supplements
Food and supplements rich in omega 3 fatty acids help reduce inflammation throughout the body, lower blood pressure, and the risk of heart attack.
- Fish and Fish Oil- are high in omega 3 fatty acids, especially in fish like salmon, herring, and tuna. Fish oil supplements are also high in omega 3 fatty acids.
- Flax and flaxseed oil- contain omega 3 fatty acids and fiber.
- Greensoul- is a natural supplement that helps to maintain a healthy cholesterol level, supports the body’s immunity, and the ability to fight free radicals.
- Coenzyme Q10- helps maintain a healthy cholesterol level, boosts immunity, and energy.
- Perfusion SR- helps enhance blood flow, maintain a normal blood pressure, and enhance the elasticity of large arteries.
Procedures to restore blood flow
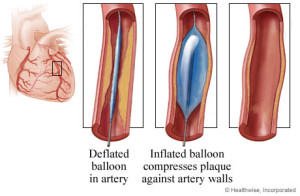
Angioplasty and stent placement: this is a procedure considered as non-surgical because it is done by Dr. Jamnadas, who accesses the artery by inserting a long, thin tube (catheter) into the narrowed part of your artery while being visualized under x-ray.
A wire with a deflated balloon is passed through the catheter to the narrow area. The balloon is then inflated, compressing the plaque against the artery wall and widening it, so it no longer restricts blood flow.
Angioplasty and stent placement Procedure
Blocked arteries supplying the heart, kidneys, legs, arms and brain can easily be treated with stenting or endarterectomy.
Unlike stenting done in the coronary arteries, only bare metal stents are used in the peripheries. Bare metal stents act as a scaffolding to keep an artery open but suffer a 30% re-stenosis rate. This is due to a process called intimal hyperplasia which is attributed to a keloid like growth. A keloid is an overgrowth of the inner lining of the blood vessel that covers over the stent.
However, this reparative process lasts no more than 6 months. After 6 months, if an artery has not re-narrowed at the site of the stent, it is unlikely to re-narrow.
If symptoms were to reoccur, it would be due to New blockages at another site within the arteries.

Stents are made of either metal or plastic.
**Patients will need to improve risk factor modifications to prevent New blockage formation.
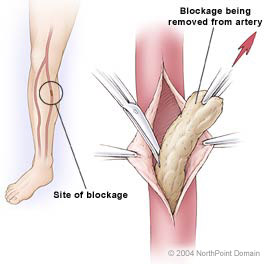
Endarterectomy: is a procedure where a catheter is used to scrape the inner lining of an artery. That material which is blocking the artery is extracted and then taken out of the artery using the catheter. The procedure is Best suited for blocked arteries in the legs. Laser atherectomy has been used in the legs also, but Dr. Jamnadas does not favor it at this time due to the high re-stenosis rate.
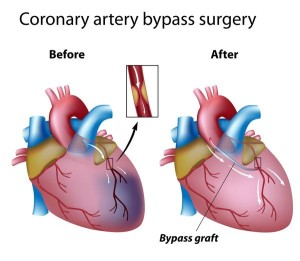
Bypass Surgery: is performed by removing a portion of a small blood vessel and sewing or ‘grafting’ one end of the bypass proximal to the area of blockage and the other end beyond the area of blockage, therefore bypassing the affected area.
How can I prevent this?
-
Do not smoke!
-
Maintain a healthy weight with a BMI <25
-
Maintain a normal blood pressure, cholesterol and sugar levels.
-
Eat nutritious, low-fat foods and avoid foods high in cholesterol.
-
Exercise regularly for 30 minutes at least 3-4 times a week.