What is Aortic Stenosis?
Aortic stenosis is a condition in which the aortic valve narrows and prevents the valve from completely opening. This restricts blood flow out of the aorta and heart. Restriction of blood flow exiting the aorta diminishes the body’s potential to receive the maximum amount of oxygen rich blood.
Over time the pressure increases in the left ventricle forcing the left ventricular wall to work harder and eventually become thicker and weaker. Weakening of the heart muscle can lead to the development of symptoms including weakness and fatigue.
What are the causes?
Narrowing of the aortic valve may be caused by the following:
- Congenital heart defects: unicuspid or bicuspid aortic valve
- Calcification
- Rheumatic fever- a condition that may develop after strep throat with valvular disease developing 5-10 years after rheumatic fever occurs
- Type II hyperlipoproteinemia
Rare causes include:
- Fabry’s disease
- Systemic lupus erythematosis (SLE)
- Paget disease
- Alkaptonuria
How does a normal heart work?
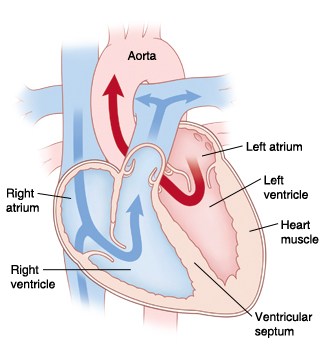
The heart consists of four chambers. The top two chambers (atria) receive blood while the bottom two chambers (ventricles) pump blood out.
Deoxygenated venous blood returns to the right atrium of the heart. Blood flows from the right atrium to the right ventricle by the opening of the tricuspid valve. Blood is prevented from going backwards into the atrium by the closure of the tricuspid valve. The right ventricle then contracts and pumps blood out through the pulmonary valve into the pulmonary artery. The pulmonary valve is closed and the blood is sent to the lungs where it picks up oxygen.
Oxygenated blood returns from the lungs by the pulmonary veins and enters the left atrium. From the left atrium, blood enters the left ventricle by the opening of the mitral valve. Blood is prevented from flowing back into the left atrium by the closure of the mitral valve. Blood is then pumped out the left ventricle to the aorta by the opening of the aortic valve. Blood is prevented from flowing back into the left ventricle by the closure of the aortic valve. From the aorta, oxygenated blood is pumped out to the entire body.
What happens in aortic stenosis?
The aortic valve consists of three leaflets (cusps) which connect to the aorta by a ring called the annulus. Heart valves only open in one direction. Once all of the blood has emptied out of the left ventricle, the aortic valve tightly closes to ensure no backflow of blood.
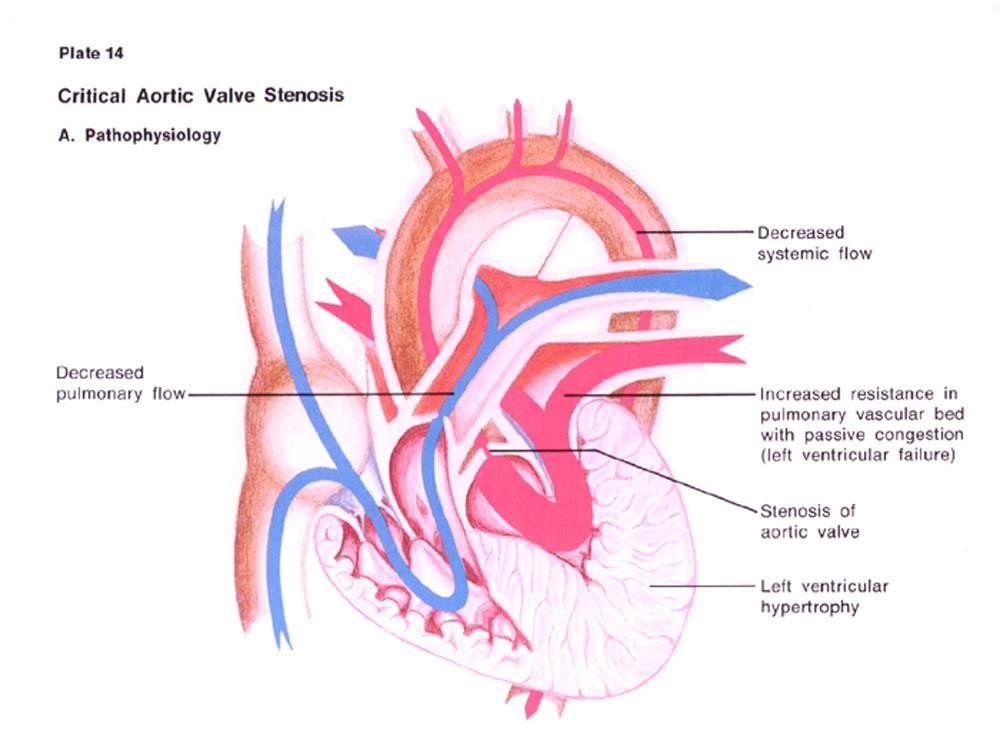
In aortic stenosis, the leaflets become thickened or calcified preventing the valve to completely open. The thickening of the leaflets make the valve opening narrowed. The ejection of blood from the left ventricle struggles to get through the narrowed opening. The complete emptying of oxygenated blood from the left ventricle is limited, increasing pressure in the ventricle and eventually thickens the wall of the left ventricle.
The limiting of blood flow into the aorta results in symptoms of breathlessness, dizziness, and loss of consciousness.
What are the risk factors?
Aortic stenosis is not considered a preventable disease, yet some risk factors include:
- Congenital abnormalities: bicuspid aortic valve (born with two aortic leaflets)
- Age: increasing age along with calcium deposits on valves
- History of rheumatic fever: causes leaflets to thicken, stiffen, or fuse
- Hypertension (high blood pressure)
- Hypercholesterolemia (high cholesterol)
- Diabetes (high glucose)
What are the symptoms?
Patients with aortic stenosis may have no symptoms at all.
Aortic stenosis ranges from mild to severe. Symptoms typically develop in severe aortic stenosis.
Symptoms include:
- Shortness of breath with activity
- Angina (chest pain)
- Fainting, weakness, or dizziness
- Fatigue
- Palpitations (sensation of feeling a rapid heart beat)
How is it classified?
Aortic stenosis is classified as:
- Mild- valve area 1.1-1.9cm2 and/or transvalvular gradient <30 mmHg
- Moderate- valve area 0.8- 1.1cm2 and/or transvalvular gradient 30-50 mmHg
- Severe- valve area 0.8- 1cm2 and/or transvalvular gradient >40 mmHg
Normal valve area: 3.0- 4.0cm2 with no transvalvular gradient
What are the complications?
Complications of aortic stenosis include:
- Angina
- Syncope
- Left ventricular hypertrophy
- Heart failure
- Arrhythmias
- Endocarditis
- Cardiac arrest
Call your doctor immediately if you have any of the following:
-
Chest pain or shortness of breath
-
Weakness in the muscles of your face, arms, or legs
-
Difficulty in speaking
-
Rapid or bounding heartbeat
-
Fainting or dizziness
How is it diagnosed?
Aortic stenosis is usually diagnosed during a routine visit with your physician.
Diagnosis is based around three parameters including patient history, physical examination, and tests.
1. Patient history
Patients may complain of symptoms in severe aortic stenosis.
Symptoms of:
- Angina
- Dizziness
- Syncope
- Loss of breath
2. Physical examination
During a routine physical examination, your health care provider will notice the following:
- Faint pulse may be felt
- Changes in the quality of pulse in the neck
- During auscultation a murmur may be heard
3. Tests
The following tests may be performed:
- Electrocardiogram (EKG) – a noninvasive test performed in our clinic which determines the electrical activity of your heart. This test may be used to detect left ventricular hypertrophy (thickening) which may occur due to aortic stenosis.
- Chest X-ray- a simple test performed in our office showing the size and shape of the heart to determine whether the left ventricle is enlarged. Also reveals the presence of fluid in the lungs which may occur due to aortic stenosis.
- Echocardiogram (ECHO)- a noninvasive test using sound waves to determine the size and function of the heart’s chambers and the structure and function of the heart valves.
- Cardiac catheterization- a hospital procedure used to diagnose the type and severity of your heart condition. A thin tube (catheter) is inserted into an artery in your arm or groin to reach the heart. A contrast dye will be given to view the arteries and seen under x-ray guidance. This allows the physician to see any abnormalities in the arteries including blockage that may coexist with aortic stenosis.
How is it treated?
Lifestyle changes are implemented in patients diagnosed with aortic stenosis to stop the progression of the disease.
Treatment of aortic stenosis is primarily done with surgical intervention, although medications can be used to relieve symptoms of aortic stenosis.
Lifestyle modifications
Lifestyle modifications help reduce the work load on the heart.
Lifestyle modifications include:
- Maintain a healthy weight with a BMI <25
- Limit salt intake
- Maintain cholesterol, sugar, and blood pressure
- Exercise for at least 30 minutes a day 5 days a week
- Stay physically active
- Do not smoke!
Medications
Medications are used to reduce symptoms and control heart rhythm disturbances associated with aortic stenosis.
Medications may be used to lower blood pressure or cholesterol.
- Cholesterol lowering medications– these act by decreasing the amount of cholesterol in blood, especially Lowering your low density lipoprotein (LDL- your Lousy cholesterol) and keep your high density lipoprotein (HDL- your Healthy cholesterol) High.
- Beta blockers- this lowers the heart rate and decreases blood pressure.
- Diuretics- these are sometimes referred to as ‘water pills’ which helps excrete excess water.
- Antibiotics- people who had rheumatic fever in the past may require long-term treatment with penicillin.
Surgical Procedures
Surgical valve repair or valve replacement is preferred in patients who develop symptoms; even if symptoms are not bad, surgery is still recommended.
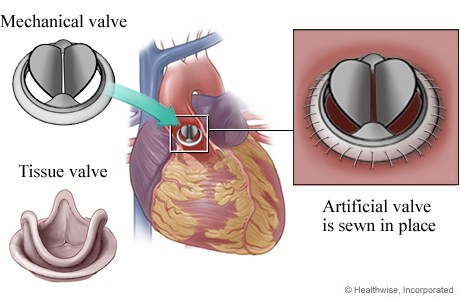
Aortic valve replacement offers substantial improvement of symptoms and life expectancy. The only effective treatment for severe aortic stenosis is aortic valve replacement.
Therapies to repair or replace the aortic valve include:
- Balloon valvuloplasty- in a hospital setting, the physician inserts a thin tube (catheter) tipped with a balloon into an artery in the leg or arm to reach the heart. The catheter is positioned into the narrowed aortic valve and the balloon-tipped catheter is inflated. The balloon pushes the aortic valve open and stretches the valve opening, improving blood flow. Balloon valvuloplasty may relieve aortic valve stenosis and symptoms, although re-stenosis of the valve is common.
- Aortic valve replacement- is the primary treatment for severe aortic stenosis. The entire aortic valve will be replaced by a surgeon. A mechanical (metal) or tissue valve (organic) may be used to replace the stenotic valve. A mechanical valve requires life-long anticoagulation therapy such as warfarin (Coumadin) to prevent blood clot formation. Tissue valves usually come from a pig or cow. Blood does not clot easily on tissue valves so patients may only need Coumadin or aspirin for only a short time. Tissue valves may wear out faster than mechanical valves and may need to be replaced sooner.
-
Transcatheter aortic valve implantation (TAVI) – this is a less invasive approach for aortic valve replacement with a prosthetic valve. The approach can be transfemoral (femoral artery in leg) or transapical (apex of heart). TAVI approach is reserved for patients who are at an increased risk of complication from aortic valve surgery.
What is the prognosis?
Without treatment, an individual with aortic stenosis with symptoms or complications may do poorly.
Aortic stenosis can be cured with surgery although there is a risk for arrhythmias (irregular heart rhythm) which may cause sudden death. There is also a risk that the new valve will stop working and may need to be replaced.
How can I prevent this?
Aortic stenosis itself often can not be prevented, although some of the complications may be prevented.
- Prevent rheumatic fever: See a physician when you have a sore throat. Treating strep infections promptly with antibiotics can prevent rheumatic fever that causes aortic stenosis.
- Reduce risk factors of coronary artery disease: Lower blood pressure, obesity, high cholesterol, and sugar. It is a good idea to maintain a healthy weight with a BMI below 25.
- Practice good oral hygiene: gum infections may also cause inflammation of the heart tissue called endocarditis.