What is Aortic Dissection?
What are the causes?
- Bicuspid aortic valve
- Marfan’s syndrome – connective tissue disease
- Cystic medial necrosis – connective tissue disease
- Ehlers- Danlos syndrome – collagen synthesis defect
- Turner syndrome – chromosomal abnormality
- Coarctation of the aorta – narrowing of the aorta
- Syphilis – infection
- Arteritis – inflammation of artery
- Pregnancy – III trimester
- Cocaine abuse
- Traumatic injury to the chest – motor vehicle accidents in which the chest hits the steering wheel
How does it occur?
Deterioration of the inner layer of the aorta is said to be a prerequisite in the development of non-traumatic aortic dissection. Following deterioration, tearing of the inner layer or aortic intima may occur.
Blood passes into the middle layer or aortic media through the tear, separating the intima from the media and dissects the blood vessel.
The dissection can spread both proximal (before) and distal (after) to the tear, involving major branching vessels of the aorta and aortic valve and filling blood around the heart.
Spread of this nature is responsible for many of the symptoms including ischemia (decrease in blood supply) to vital organs, aortic regurgitation, and cardiac tamponade.
Who is at risk?
- Sex: men are at higher risk compared to woman
- Age: ages between 60s and 70s
- Uncontrolled hypertension
- Atherosclerosis
- Pre-existing aortic aneurysm
- Bicuspid aortic valve
- Aortic coarctation
- Turner’s syndrome
- Marfan syndrome
- Loeys-Dietz syndrome
What are the symptoms?

- Sudden severe chest pain in chest or upper back, described as tearing, ripping, or shearing
- Loss of consciousnessChestPain
- Shortness of breath
- Profuse sweating
- Sudden difficulty in speech, vision, or paralysis of half of the body
- Confusion or disorientation
- Weak pulse compared to other arm
- Dizziness
- Nausea and vomiting
What are the types?
Illustration of Type A vs Type B
What are the complications?
- Death due to massive internal bleeding
- Organ damage
- Insufficient circulation past the area of dissection
- Thrombosis
- Heart attack
- Stroke
- Cardiac tamponade
- Aortic regurgitation
How is it diagnosed?
The diagnosis of aortic dissection is based on three parameters including patient history, physical examination, and tests.
1. Patient history
-
Sudden severe tearing or ripping pain in the chest or back
-
Disorientation or confusion
-
Profuse sweating
2. Physical Examination
-
Delay in pulse between arms and legs
-
Hypertension or hypotension
-
Blood pressure difference between right and left arms
-
Auscultation over the chest may reveal a “blowing” murmur
-
New stroke symptoms and signs like decreased sensation or movement

Example of a Chest X-ray
3. Tests
-
Chest X-ray: reveals widening of the mediastinum X-ray of an aneurysm
-
Transesophageal echocardiogram (TEE) – a test that uses high pitched sounds to produce images of the heart by passing a probe down the esophagus to view the heart
-
Computerized tomography (CT) scan: injection of a contrast dye is used to visualize the aorta
-
Magnetic resonance angiogram (MRA) – uses magnetic fields to form images of the body
How is it treated?
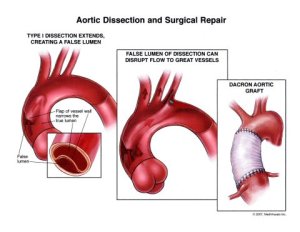
Aortic Dissection and Surgical Repair
What is the prognosis?
Aortic dissection is life threatening. The condition can be managed with surgery if it is done before the aorta ruptures. Less than half of the patients with ruptured aorta survive.
For Type A aortic dissection, the mortality rate remains high, with up to 30% deaths after surgery.
For Type B, when treated medically, the mortality rate is less with a death rate of 10%.
In both types, the ten year survival rate is more than 60%.
How can I prevent this?
- Controlling blood pressure, diabetes, and cholesterol
- No smoking
- Maintain a healthy weight with a BMI <25
- Wear a seat belt
- Continue taking the medications prescribed to you
- Any chest pain should not be ignored and medical care should be given immediately by emergency medical services and calling 9-1-1

