What is an Abdominal Aortic Aneurysm?
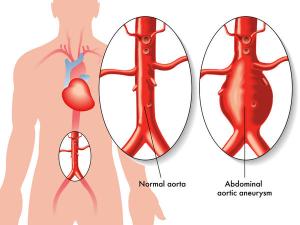
An abdominal aortic aneurysm (AAA) is a permanent local dilatation or bulge in the aorta greater than 1.5 times its normal diameter.
The aorta is the largest vessel carrying blood from the heart to the rest of the body. The aorta leaves the heart and descends through the chest and abdomen until it splits into two arteries to supply the legs.
The aorta is an elastic structure which is capable of loosing its elasticity as it gets further away from the heart. Therefore the most common site for an aneurysm is in the abdomen. Most aneurysms have a spindle shape, but the size, shape, and extent varies in patients.
When there is a weakening in the walls of the aorta, the high pressures within the vessel cause a bulge or sac. Further weakening of this sac and enlargement can lead to a rupture of this major blood vessel causing severe bleeding. A ruptured aneurysm requires emergency management.
Blood tends to collect within these sacs which may lead to clot (thrombus) formation. If this dislodges from the sac, it can travel to other areas of the body and obstruct circulation to a particular area.
What are the causes?
- Congenital causes: born with a genetic predisposition to a weakness in the artery walls
- Family History: AAA may have a tendency to run in families
- Inflammatory causes: arteritis (inflammation of the arteries)
- Infective causes: syphilis or fungal infections
- Trauma
Abdominal Aortic Aneurysm
What are the risk factors?
- Sex: men are more commonly affected than women
- Age: ages 60-65 and increasing age
- Race: Caucasians have a higher risk than African Americans
- Smoking
- Family history of AAA
- High blood pressure (hypertension)
- High cholesterol
- Diabetes
Who needs to be screened?
- Men between the ages of 65 to75 with a history of smoking
- Men aged 60 and older with family history of AAA
- Both men and women with risk factors of AAA
What are the symptoms?
Most abdominal aortic aneurysms are small and have no symptoms. Most people are unaware of it and are often discovered as an incidental finding during work-ups for other problems.
Symptoms are produced as aneurysms grow. The most common symptom of an abdominal aortic aneurysm is pain that may be felt in the abdomen, back, or groin.
A sudden and very severe abdominal, back, or groin pain may indicate a rupture of the aneurysm. A ruptured aneurysm requires emergency management.
How is it diagnosed?
Diagnosis is based around 3 parameters. These parameters include: Patient History, Physical Examination, and Imaging tests.
Patient History:
-
Symptoms of pain in the abdomen, back, or groin
- Symptoms of claudication (pain while walking) in both of the legs may indicate an occlusion in the abdominal aorta
- A patient may complain of a swelling located in the abdomen
Physical Examination:

- During a physial examination, your vitals will be taken. Vitals include your pulse, blood pressure, and temperature. High blood pressure is an indication for further work up.
-
An aneurysm may be felt in the abdomen as a small soft pulsating mass around the navel.
-
Peripheral pulses will also be checked to determine if an associated aneurysm or occlusive disease is present.
-
A stethoscope is placed over the abdomen to listen for a whooshing sound called a bruit.
Imaging tests
Imaging tests are performed to determine the size, location, and extent of an aneurysm. This also helps assess the risk of rupture and management.
- Abdominal Ultrasound- is a simple, non-invasive office procedure used to view images of the abdominal aorta.
- Magnetic Resonance Angiography (MRA) – this is a test similar to an MRI, which involves a contrast dye to be injected into a vein, while pictures are taken of the aorta.
- Computerized Tomographic (CT) Angiography: this test also involves the injection of a dye into the vein while pictures of the aorta are taken.
- Angiography: This is an invasive test done in a hospital setting, involving the insertion of a thin catheter into the groin which is then advanced up to the aorta. A contrast dye is given to view the aorta and seen under x-ray guidance. This shows the location and extent of an aneurysm.

Example of a Magnetic Resonance Angiography (MRA)
How is it treated?
Treatment includes preventing the progression of growth and preventing complications.
Treatment involves three separate parameters including: lifestyle changes, medications, and procedures.
Lifestyle changes
- First line of treatment is to reduce the risk factors by diet changes, exercise, and weight management.
- Eat foods high in fiber such as whole grain cereals, oatmeal, and figs. Eat plenty of fruits such as apples, bananas, prunes, oranges, and pears. Include fish and legumes such as beans or chickpeas.
- Lower your salt intake
- Avoid fatty foods including bad saturated fat that is found in some meats, dairy products, chocolates, baked goods, and deep-fried food.
- Maintain a healthy weight with a BMI below 25
- No smoking
- Be more physically active
- Relax and reduce stress
Medications:
- Beta Blockers– to lower the blood pressure within the vessels.
- Cholesterol lowering medications– these reduce cholesterol levels in patients with atherosclerosis.
- Aspirin – prevents platelets from clumping together. This reduces the chances of a blood clot from forming and narrowing or obstructing the arteries. This is not appropriate for all patients including patients with bleeding disorders or those already taking a blood thinner.
Procedures:
- Open surgery
- Endovascular repair
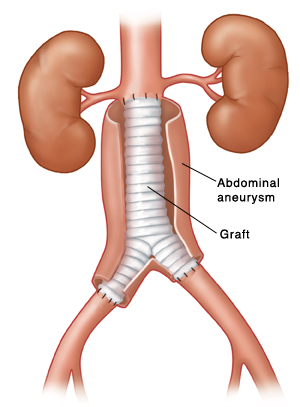
Open surgery- is a definitive treatment for symptomatic and high risk patients. This operation is done under general anesthesia and can last 4-6 hours. The abdomen is opened and a section of the aorta is removed. This section is replaced with a graft and the graft is covered by the artery wall and sutured into place.
Following this, normal blood flow is ensured. All surgeries carry a risk, although this holds a definitive treatment for aneurysm repair.
Endovascular repair- is a less invasive procedure which involves the placement of a stent within the abdominal aorta. A catheter is inserted into the groin through a small incision and advanced up to the aorta. A contrast dye is given to view the aorta and seen under x-ray guidance. A metal stent is positioned in the aorta which acts as a scaffolding for the artery.
Although this is less invasive, this is not a definitive treatment.
Who is not eligible?
- Severe COPD
- Severe heart disease
- Active infection
- Severe co-morbidities including cancer or other end-stage diseases
What are the risks of surgery vs. the risk of rupturing?
- The size and rate of growth of the aneurysm
- Symptoms
- Multiple aneurysms present
- Surgical risk
What are the complications?
- Inflammation
- Infection
- Aorto-venous fistula- an abnormal connection between the aorta and a vein
- Aortoenteric fistula- an abnormal connection between the aorta and bowel
- Thromboembolism- dislodged clot with the potential to obstruct or narrow a vessel
- Excruciating pain
- Severe hemorrhage (bleeding)
- Low blood pressure
- Shock
- Death
What is the prognosis?
Most abdominal aortic aneurysms grow slowly. If the aneurysm is slow growing, the prognosis is good.
Increasing size on an aneurysm increases the chance of rupture. The prognosis is good for patients who undergo aneurysm repair.
However, a ruptured abdominal aortic aneurysm holds a bad prognosis. Less than 80% of patients survive a ruptured aneurysm of such a major vessel.
How can I prevent this?
- NO Smoking
- Controlling high blood pressure, cholesterol, and diabetes
- Eating a healthy diet
- Keeping physically active regularly with the right kind of exercise
- Maintain a healthy weight with a BMI <25
- Reduce stress!
|
FOOD ITEM |
GI |
FOOD ITEM |
GI |
| White bread |
71 |
Broad beans |
79 |
| Golden Grahams |
71 |
Jelly beans |
80 |
| Millet |
71 |
Pretzels |
81 |
| Watermelon |
72 |
Rice Krispies |
82 |
| White rolls |
73 |
Potato, microwaved |
82 |
| Puffed wheat |
74 |
Cornflakes |
83 |
| Corn chips |
74 |
Potato, instant |
83 |
| Chips |
75 |
Potato, baked |
85 |
| Waffles |
76 |
Rice pasta, brown |
92 |
| Doughnut |
76 |
Baguette |
95 |
| Wafer biscuits |
77 |
Parsnips |
97 |
| Rice cakes |
77 |
Dates |
103 |
| Weetabix |
77 |