What is Ventricular Fibrillation?
Ventricular fibrillation is an abnormal heart rhythm that occurs when the heart beats so rapidly and irregularly that the heart muscle quivers and does not beat at all.
In ventricular fibrillation, the ventricles produce many abnormal circuits, instead of following the normal electrical pathway from the atria down to the ventricles. This usually occurs due to damaged heart muscle.
The ventricles beat very quickly and irregularly, so blood is not pumped out of the heart to vital organs of the body. If the heart is not able to pump at all (cardiac arrest), death may occur if emergency treatment is not given to return the heart rhythm to normal.
Animation of Ventricular Fibrillation
How does ventricular fibrillation occur?
In ventricular fibrillation electrical impulses can become chaotic after the heart muscle has been damaged. Damage usually occurs after a first heart attack or due to problems from a scar in the heart muscle from a previous heart attack. Electrical activity is not passed through these scarred areas. The ventricles begin sending out their own rapid and chaotic impulses and take over the pacemaker function of the SA node.
Ventricular fibrillation may also develop if ventricular tachycardia is left untreated.
Rapid, chaotic electrical impulses cause the ventricles to quiver instead of pumping the blood out of the heart. This causes low blood pressure and no blood supply to the vital organs of the body including the brain. Most people lose consciousness within seconds and require immediate cardiopulmonary resuscitation (CPR).
The survival rate in ventricular fibrillation is better if CRP is initiated immediately until the heart can be shocked back into rhythm with the use of a defibrillator. If these measures are not taken immediately, death can occur within minutes.
What are the causes?
Ventricular fibrillation is usually caused after damage to the heart muscle from a previous heart attack.
Ventricular fibrillation can occur whenever the heart does not receive enough oxygen or due to abnormalities or diseases of the heart, or by diseases elsewhere in the body affecting the heart. Ventricular tachycardia may occur after open heart surgery, substance abuse, or medications.
Heart abnormalities and diseases include:
- Congenital heart defects (heart defect from birth)
- Coronary artery disease (decreased blood supply to the heart) or atherosclerosis
- High blood pressure
- Heart attack
- Cardiomyopathy and congestive heart failure
- Rheumatic fever and pericarditis (inflammation of the heart)
- Abnormalities of the heart valves, especially mitral stenosis and mitral regurgitation
- Hypertrophy (enlarged heart)
Diseases elsewhere in the body affecting the heart:
- Hyperthyroidism
- Pulmonary embolism (blood clot in lung)
- Chronic obstructive pulmonary disease (COPD) and emphysema
- Sleep apnea
- Electrolyte imbalances (low potassium/ magnesium levels)
Substance abuse:
- Consuming large amounts of alcohol (binge drinking)
- Cocaine, amphetamines, diet pills, caffeine, or cold medicines
- Tobacco
- Carbon monoxide intoxication
Surgery
First week following open heart surgery
Medications
Amiodarone
Sotalol
Who is at risk?
Several factors may increase the risk of ventricular fibrillation.
These include:
Men
Increasing age
Congenital heart disease
Family history of ventricular tachycardia or ventricular fibrillation
Previous episode of ventricular fibrillation
Previous heart attack
Hypertension
Excessive alcohol consumption
Electrolyte imbalance
Heavy caffeine use
Smoking
Substance abuse i.e. cocaine
Heart failure patients and COPD patients
Pericarditis (inflammation of the heart) and autoimmune diseases
Other chronic conditions including thyroid disorders and sleep apnea
What are the symptoms?
An episode of ventricular fibrillation presents with unconsciousness or sudden collapse. This is due to a lack of oxygen rich blood to the brain and other vital organs.
The following symptoms may occur within 1 hour before the collapse:
Chest pain
Dizziness
Nausea
Rapid heartbeat (tachycardia)
Shortness of breath
When should I seek medical care?
If you experience symptoms of ventricular fibrillation, seek emergency care immediately.
If you faint, have difficulty in breathing, or have chest pain lasting more than a few minutes, call emergency care or call 911. These are urgent symptoms of a life-threatening ventricular fibrillation and must seek emergency care immediately to avoid the risk of cardiac arrest and death.
Steps to follow:
Call 9-1-1
Cardiopulmonary resuscitation must be initiated immediately from someone trained in CPR. This can be given by a family member or medical personnel. Chest compressions (30) must be started immediately followed by rescue breaths (2). This cycle is to be repeated until a shock or defibrillator can be given.
What are the complications?
The most common complication of ventricular fibrillation is sudden death. This occurs within 1 hour of symptoms.
Complications in those who survive include:
Neurological damage
Reduced mental perception
Coma
How is it diagnosed?
Ventricular fibrillation is a medical emergency and is not typically diagnosed before hand unless an episode of collapse occurs within the doctor’s office.
Your physician will know if you are in ventricular fibrillation based on history, physical examination, and tests.
1. History
The patient will give history of sudden loss of consciousness or collapse.
History of warning symptoms of fibrillation may be given such as chest pain, dizziness, nausea, fast heart rate, or difficulty in breathing.
2. Physical Examination
After collapse:
Unconscious patient
Before collapse:
Weak or no pulse
Low blood pressure
Rapid breathing
Varying heart sounds heard over chest
3. Tests
Certain tests can be performed to determine the cause and severity of your condition including:
Blood tests- to check potassium, magnesium, and thyroid hormone levels and certain cardiac enzymes
Electrocardiogram- this is a very useful and simple test that records the electrical activity of the heart and reveals ventricular fibrillation. Also shows signs of heart attack, conduction abnormalities, hypertrophy, and electrolyte imbalances.
Chest X-ray- a simple test performed in our office showing the size and shape of the heart. Also reveals the presence of fluid in the lungs.
Echocardiogram (ECHO) – a noninvasive test performed in our office to determine the size and function of the heart’s chambers and the structure and function of the heart valves.
How is it treated?
Ventricular fibrillation is a medical emergency and must be treated immediately.
The goal of treatment is to restore blood flow as quickly as possible to prevent damage to vital organs.
Once blood flow is restored, treatment is given to prevent future episodes.
Cardiopulmonary Resuscitation (CPR) – this mechanically helps to restore blood flow to vital organs by mimicking the pumping action of the heart.
– Call for emergency help immediately.
– CPR can be performed by anyone trained in CPR including a family member until medical personnel arrives.
– As per new regulations, chest compressions must be initiated first rather than giving rescue breaths. Count 30 chest compressions that must be given hard and fast (at a rate of 100 beats per minute) over the chest. Allow the chest to rise completely between compressions.
After 30 chest compressions are given, mouth-to-mouth breathing must be given with 2 rescue breaths with the person’s neck in an extended position to allow airflow through the airways.
Repeat chest compressions and rescue breaths until help arrives.
Defibrillation- this is a device used to deliver a quick electric shock through the chest wall. This is given to ‘shock’ the heart out of the chaotic rhythm and usually allows the heart to resume a normal heart rhythm.
A shock may be given by medical personnel or may be given through a public-use defibrillator. A public defibrillator can be located in public places including airports, schools, malls, and community centers. A public defibrillator is called an Automated External Defibrillator (AED).
Once a person collapses and CPR is initiated, an AED must be retrieved. Turn the device on by pushing the power button. In the AED kit, two pads will be provided that must be matched up accordingly to the areas over the chest to the pictures given on the pads. The device will detect if the heart is to be shocked or not. If the heart requires a shock, stand clear and press the “Shock” button. CPR must be resumed until help arrives or until the person begins to move.
It is important to take a CPR class especially in those with family members who are at risk.
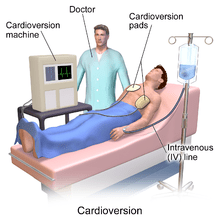
Illustration of Cardioversion procedure.
Cardioversion: a medical procedure that restores a normal heart rhythm in people with certain types of abnormal heartbeats (arrhythmias). if pulse is present, in a hospital setting a shock is delivered to your heart through pads attached to the chest wall. The current interrupts the electrical impulses in the heart and restores a normal rhythm.
Treatment to prevent future episodes
If structural damage has occurred in the heart after ventricular fibrillation episode, medications or a medical procedure may be recommended to reduce the risk of a future episode.
1. Medications
Various anti-arrhythmic drugs may be used in the long term treatment of ventricular fibrillation.
Different classes of medications may be used including beta blockers, angiotensin-converting enzyme (ACE) inhibitors, calcium channel blockers, and anti-arrhythmics (amiodarone).
Since there is a stagnation of blood in the heart during fibrillation, blood clots commonly develop in the heart. Medications are used to prevent the formation of blood clots.
These drugs include:
Heparin
Warfarin
Dabigatran
Aspirin
Clopidogrel
2. Implantable cardioverter-defibrillator (ICD)
An implantable cardioverter-defibrillator (ICD) is a device that detects any life-threatening, rapid heartbeat. After fibrillation has been stabilized, an ICD implantation may be recommended.
This is a small implantable device used to detect abnormal heart rhythms and shock the heart out of the dangerous rhythm.
Animation of an ICD
3. Catheter ablation:
is a hospital procedure done to destroy areas on the heart that are causing irregular heart rhythms.
A thin flexible tube is inserted into a blood vessel to access the heart. Heat is applied to the tip of the catheter to permanently destroy small areas of abnormal heart tissue.
The damaged tissue is no longer capable of generating electrical impulses.
What is the prognosis?
With early detection and effective CPR given before a defibrillator is given, up to 25% of victims are able to leave the hospital without neurological damage.
If ventricular fibrillation occurs within the hospital with a heart attack, defibrillation has a 95% success rate.
If shock and heart failure occur, even with defibrillation only 30% of those shocked will return to a normal heart rate.
The survival rate for a person who has an attack of ventricular fibrillation outside the hospital ranges between 2-25%.
How can I prevent this?
Ventricular fibrillation can not always be prevented, but there are ways of reducing the risk of developing ventricular fibrillation. Leading a healthy lifestyle may reduce the chance of coronary artery disease, which can cause ventricular tachycardia and fibrillation.
Some ways you can reduce the risk is by:
No smoking!
Drink in moderation
Limit caffeine
Avoid recreational drugs
Be physically active. Engage in moderate physical activity for at least 30 minutes a day
Eat nutritious foods low in cholesterol and fats
Maintain a BMI below 25
Control high blood pressure, cholesterol, and sugar
Control stress
Have regular physical exams and report any signs or symptoms to your physician.
Take a CPR course if a family member or friend is at risk of ventricular fibrillation.